
This article has an erratum available at: http://dx.doi.org/10.21037/aes-2024-01 the article has been update on 2024-09-03 at here.
Making the case for the evolving role of social media in health professions education and a literature review on the application of some in ophthalmology
Introduction
Technology has enabled learners to become content creators and use their content in online learning environments for collaboration, interaction, and engagement. Social media (SoMe), in particular, can help us to connect with content, information, and people to meet ongoing lifelong learning needs. It is widely embedded in our daily lives, used for practicalities, and is easily accessible and user-friendly. SoMe can be defined as Internet-based applications on which people create and share content, and build social networks (1).
SoMe can be used as a resourceful platform offering networking and learning opportunities whereby communities of learning may organically emerge, enabling their members’ professional identity development while engaging collaboratively in their mutual field of practice. SoMe may be embedded in traditional online or in-person educational programs and scale the learning experience beyond time and geographical constraints involving a wider and more diverse learning community. In SoMe, people create online personal profiles, which become tagged to their virtual creations and interests, blend with content, and enable networking with other digital objects and people sharing mutual goals. People can express themselves and interact by sharing, liking, and commenting using diverse ways of communication such as text, images, sound, and videosJeny (2).
Research confirming the applicability and effectiveness of SoMe in Health Professions Education (HPE) is scarce. A review of 14 selected studies by Cheston et al. (3) in 2013 shows that SoMe may enable competency improvement and provide opportunities for learner engagement (71%), feedback (57%), collaboration, and professional development (36%). Technical issues (43%), variable learner participation (43%), and privacy/security concerns (29%) were noted as challenges. Based on 698 papers, Chan et al. (4) acknowledged a ubiquitous and steady increase in the use of SoMe in HPE. SoMe strategies were categorized as (I) push-based, with occasional engagement opportunities such as blogs, podcasts, and organizations’ SoMe accounts; (II) interaction-based such as Twitter journal clubs/chats, Facebook groups, WhatsApp-based teaching/discussions, and online virtual community of practice (CoP); and (III) blended by combining both, such as live tweeting conferences and virtual networking and mentorship. Online social networking engagement of learners with peers and educators helps elevate self-esteem, motivation, and academic success (5).
Sterling et al. (6) underscored the importance of conducting more comprehensive research to better understand the impact of SoMe on postgraduate medical education, recruitment, and professionalism as the quality of existing studies is modest at best.
Guckian et al. (7) emphasized the positive impact of SoMe on medical students associated with communication improvement with educators and with both objective and self-reported learning improvement. On the other hand, they noted a lack of clear evidence regarding long-term retention of knowledge and occasionally negative impacts on mental and physical health.
He et al. (8) investigated how ophthalmologists used SoMe for their personal and professional development at the height of the coronavirus disease 2019 (COVID-19) pandemic. Ninety-four percent reported having a professional SoMe account, most frequently Instagram (25.2%), LinkedIn (22.6%), and Facebook (19.6%). Most participants (64%) declared spending at least 1 hour daily on SoMe to connect with family, promote professional services, educate patients, share clinical cases with colleagues, and find mentorship and networking opportunities.
As learners and educators have been challenged to adopt new technologies, opportunities for innovation in HPE have appeared and SoMe emerged as a field of scholarship, deserving further investigation. Thus, we conducted a review of recent literature on this topic, summarized the most relevant theories of learning underpinning SoMe, described the depths of integration of SoMe in HPE, enumerated best practices to embed SoMe in instructional design, and addressed the role and relevance of SoMe in ophthalmology. We present this article in accordance with the Narrative Review reporting checklist (available at https://aes.amegroups.com/article/view/10.21037/aes-23-74/rc).
Methods
Our article stems from our participation as faculty in the online Teaching Skills Series of the Ophthalmology Foundation (9,10). To draw an overview of SoMe in HPE, we elected four landmark reviews (3,4,6,7). To highlight the role of SoMe in ophthalmology education, we conducted a literature review in PubMed and retrieved 160 articles from which 110 were rejected for not being related to the topic (SoMe and ophthalmology), not English written, or no abstract available (Table 1).
Table 1
| Items | Specification |
|---|---|
| Date of search | January to February 2024 |
| Databases searched | PubMed |
| Search terms used | “Social media” AND “Ophthalmology education” |
| Timeframe | Last 10 years |
| Inclusion criteria | All articles, regardless of type, in English and with abstracts available |
| Selection process | H.P.F. and K.G. conducted the search and selection |
Learning theories sustaining the role of SoMe in learning
While social learning theory states that behaviors can be acquired through observation, constructivism asserts that knowledge is actively constructed, either individually or socially. Constructivism is a social theory of learning involving observation and an active cognitive constructive process (11). Bandura explained that learning is not a simple process of knowledge translation but a mental process considering the learner’s previous experiences and the social context. People learn from one another by observing, experimenting, and modeling in a social context. SoMe creates rich social learning environments and exposes users to various points of view feeding their curiosity and providing new meanings by interacting with others experienced in their selected and/or emerged fields of interest.
Kolb argues that learning occurs through experience and is supported by reflection that generates new knowledge and skills, leading to abstract conceptualization and subsequent active experimentation. Experiential learning theory describes the learning process with concepts that support learning through SoMe. Reflection is critical to learning by observing and experimenting (12). Specific contexts shape an individual’s experience differently; past histories, learning strategies, and emotions influence the learning developed through reflection on experience (13,14). SoMe platforms, such as blogs and microblogs like X, former Twitter, can provide such virtual environments enabling individual and collective reflection. When critical reflection involves challenging perspectives beyond measuring pre-set outcomes, learners can engage in reflective problem-solving as part of transformative learning.
Focusing on the importance of the social context and sustained motivation, Vygotsky asserts that meaning is contextualized and created through social collaboration and guidance. A more experienced person, the “knowledgeable other”, i.e., an educator or coach, manages the social context and encourages and guides learners to advance experiential learning to the next level of development, designated as the zone of proximal development (ZPD) (15). The socio-cultural environment is understood as a relevant component in enhancing or limiting cognitive development.
Connectivism and heutagogy emphasize technology as the scaffold to connect and build relationships to create knowledge. Connectivism has been labeled the social constructivism of the digital age. Connections support the creation of dynamic social networks that are based on internet profiles of individuals and communities and reflect mutual goals and shared content. Knowledge becomes distributed across digital networks, and learning includes the ability to build and navigate networks, by connecting fields, concepts, and people. The “knowledgeable other” may also be found in peers, online resources, and information. Educators and learners assume interchangeable roles, and decisions about who to connect with and what to learn become a learning process (16).
Compared with pedagogy and andragogy, heutagogy (17) includes the most autonomous and self-efficacious learner (18). Instead of simply completing teacher-assigned tasks, learners are encouraged to seek areas of uncertainty and complexity in the subjects they study. Hase and Kenyon (19) proposed the designation of self-determined learners for those developing self-efficacy, applying their competencies in novel situations, and creating new ideas by actively weaving networks of knowledge and people. Self-determined learners build their own online learning environments. They set outcomes, explore, create, connect, collaborate, and reflect.
Co-constructing knowledge can stem from casual exchanges of ideas while networking, which may produce partnerships and problem-solving (20). A CoP has been conceptualized as a group of people with common interests who share their unique experiences and contributions to deepen knowledge and expertise through ongoing interactions (21). SoMe links people and information together, and supports ongoing interactions and virtual CoPs (22,23).
Learning by creative problem-solving can, also, be supported by the theory of diffusion of innovation. SoMe-based peer networking may lead to a critical mass of adopters through the influence of innovators driving novel educational strategies. Implementing a new educational idea can be explored following this theory: communicate it widely, encourage interest, review the strategy, try it, and adopt it to meet learning needs (24).
Integration of SoMe in learning and teaching
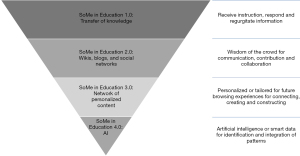
SoMe can be integrated into education across its several stages of evolution. Gerstein model (25) and the four developmental stages of the web match the evolution of technology to meet the evolving philosophies of education (Figure 1).
They are described as follows:
- In Education 1.0, learners are treated equally, regardless of their interests or previous experiences. Knowledge is transferred unidirectionally from instructor to learners as depicted by the 3 Rs—learners receive by listening and responding by taking notes and regurgitating the information previously instilled. The learning experience is educator-centered in all interactions. In this context, SoMe serves as a platform for available information.
- In Education 2.0, learners become knowledge builders within a constructivist and andragogical approach to learning. Learners interact with peers, educators, and didactics by communicating, connecting, and collaborating (3Cs). They re-use content in different contexts for additional purposes. The foundations of andragogy relate to Web 2.0, and the definition of Education 2.0 lies in humanistic roots emphasizing the importance of prior experience and social context. Social networks, wikis, and blogs epitomize Web 2.0 tools (26). Educators are learning facilitators, “guides on the side”, as opposed to “sages on the stage” (27).
- Education 3.0 embodies a heutagogical philosophy defined by significant learner autonomy and a connectivism approach that relies on building knowledge and weaving networks supported by technology. Capable, and self-efficacious, learners master their learning pathway and generate content adding value to the field of study. Web 3.0, or the semantic Web, links with the conceptualization sustaining Education 3.0. Learners can create their digital personal learning environments. SoMe may be regarded as a learning partner by pushing contextualized information and linking people with common goals. Learners connect, create, and construct (3 Cs) various intertwined social networks. Learners and educators should embrace the concept that “one can grow, change, and be significant”.
- SoMe in Education 4.0 poses a novel learning environment where learners interact across networks and lead by influence. Learners need to develop problem-solving skills and critical thinking to interact with artificial intelligence. The challenges require agility and adaptability to showcase initiative and entrepreneurialism. Content developers need to embrace effective oral and written communication. As information develops continuously, educators must access and analyze data with curiosity and imagination (28).
Incorporating SoMe in HPE has benefits to both learners and educators, such as improving communication, knowing learners through their profiles, hosting collaborative and enjoyable learning experiences, enabling behavior modeling and autonomy, nurturing content creation, and taking active roles in CoPs (29,30).
A few challenges remain for SoMe integration into the instructional design of HPE, such as ensuring the quality and accuracy of information, maintaining a significant presence, dedicating time to monitoring SoMe, protecting data privacy, maintaining professional standards to avoid cyberbullying, keeping patient-physician boundaries, and complying with regulation requirements (16-18).
Several strategies to leverage SoMe in instructional design have been proposed. In the planning stage, educators and learners should reflect on their digital identity and goals for using SoMe, and apply evidence-informed techniques, existing guidelines, shared norms, and co-creation approaches to improve HPE quality. SoMe tools and strategies should be aligned to achieve desired outcomes. During SoMe implementation, a team approach is paramount to manage an organizational SoMe presence and protect participants by defining boundaries and privacy settings. Incorporating ongoing learners’ SoMe interaction into the classroom conversation is a useful educational tool. Educators can establish SoMe as an informal backchannel where they demonstrate responsible and meaningful use. Personal and professional SoMe accounts should be separated (3,16,31).
Key elements for successful integration of SoMe in HPE
Beyond its original purpose and driven by the recent pandemic, SoMe became a dominant vehicle for discourse, debate, and education (19). Helpful SoMe practices in HPE include four critical factors to improve the educational experience by promoting communication, critical thinking, and independent inquiry (Table 2).
Table 2
| Critical factors | Description |
|---|---|
| Design of the learning experience | Curricula can be synchronous, asynchronous, hybrid, or blended. Well-designed learning environments enable participants to develop meaningful dialogue and share educational resources (20) |
| The role of the educator | Educators should act as facilitators, curators of content, amplifiers, role models, mentors, guiding learners and catalysing the learning journey towards the accomplishment of the goal and established objectives |
| Selection of SoMe platforms | This selection impacts the depth of the educational experience. SoMe platforms and tools should be specifically chosen for social networking, professional networking, media sharing, microblogging, knowledge aggregation, free open access medical education or game learning environments (16,21,24,25) |
| The purpose of the learning experience | The goal of the learning experience should guide the choice of the SoMe platform and tools that may aim: to create or support CoPs; aid in formation of professional identity; to receive, exchange, seek, create, store and organize content; or to use as a communication channel (11) |
SoMe, social media; CoP, community of practice.
When designing the learning experience, we should consider whether the learning will occur synchronously or asynchronously. When designing live learning experiences, educators and curricula designers can start with asynchronous opportunities to interact with didactics, faculty, and peers with ice-breakers, and initiating conversation (32). Optimal synchronous learning environments offer opportunities for dynamic interaction and SoMe can support dialogue, and resource exchange, and strengthen social interactions. This approach highlights the importance of community, culture, and context in knowledge construction. SoMe may also extend learning engagement with learning reinforcements after the synchronous phase (7).
The educator’s role might include additional responsibilities to maximize the effect of embedding SoMe in their educational programs. Educators act as content curators, create tutorials, adjust weekly activities with the course flow, and may amplify their impact by highlighting essential ideas or concepts using blogs or microblogs such as X. They serve as role models by using tools and activities to maintain an online presence by sending regular newsletters and stimulating activity in forums, podcasts, and weekly live sessions in synchronous platforms.
The selection of tools or platforms impacts the quality of the learning experience. Web 2.0 tools (33) can be categorized by function, such as (I) social networking like Facebook, Google Plus, and X, (II) professional networking using LinkedIn, media sharing such as YouTube, Vimeo, Instagram, and, (micro)blogs, and (III) knowledge aggregation through wikis, free open access medical (FOAM) education, and gaming environments (21,24). Each tool has advantages, disadvantages, and intended purposes (25).
The purpose of including SoMe can be to support developing CoPs, and enable educators to advance their practice by increasing peer visibility, a sense of belonging, and collective ownership associated with professional identity development (17). Lahiri and Moseley (34) developed a checklist to reflect on the overarching purpose and both social cognitive and constructivist perspectives of including SoMe in educational programs.
SoMe in ophthalmology
SoMe has emerged as a transformative force in ophthalmology, profoundly impacting practice, research, education, training, patient engagement, and enhancing clinical care (35). Its applications span from promoting ophthalmic services, enriching conference experiences, disseminating cutting-edge research literature, serving as a platform for teaching ophthalmology at medical schools, recruiting future ophthalmologists, advocating for eyecare, and facilitating collaborative endeavors (36-42).
SoMe platforms used in medical education can be grouped by function and to maximize their impact selected accordingly based on their main purpose (29). Platforms like Facebook, X, and WhatsApp serve as dynamic hubs for HPE networking and collaboration, through which ophthalmologists share insights, discuss challenging cases, and access educational resources with professional development. WhatsApp enacts collaboration, problem-solving and networking (43-48). Podcasts, encompass storytelling and trend towards sharing practical advice and new technologies. Instagram has emerged as a potent platform for education and professional visibility as well as platforms for sharing surgical videos such as Youtube and TikTok (45,49-53).
As residency programs increasingly leverage SoMe for recruitment and educational purposes, the presence of ophthalmology trainees on these platforms continues to expand (54).
Patients increasingly turn to SoMe for information about ophthalmology. This highlights the importance of implementing two-way messaging systems to improve patient care. By engaging with patients through SoMe, ophthalmologists can deliver timely postoperative instructions, enhance medication adherence and address concerns with patient outcomes. This leads to increased patient satisfaction (55-57).
SoMe has been used to share information among eye care professionals, the academic community and the public about keratoconus (58), oculoplastic (36,42,59), keratoplasty (60), cataract surgery (61), refractive surgery (62), ptosis (63), intravitreal injections (64), diabetic macular edema, glaucoma (65-67), dry eyes (68), ptosis (63), retina (69,70), strabismus (71), uveitis (72), multifocal intraocular lenses (73), refractive surgery (62), retina (74), retinopathy of prematurity (75), contact lenses (76), pediatric cataract surgery (56), diabetic macular edema (77).
The widespread use of SoMe in ophthalmology also presents challenges, particularly regarding the reliability of medical information (78). As patients and ophthalmology trainees rely more on SoMe medical content, it becomes imperative to ensure accurate information dissemination (79,80). Establishing formalized SoMe policies within training programs is essential to guide responsible usage and uphold professional standards. Regulatory bodies and healthcare organizations can play a crucial role in this effort by collaborating with ophthalmologists to establish guidelines and implement measures to regulate and monitor SoMe content (81,82). While utilizing SoMe in ophthalmology, professionals should consider the required time, the inherently public nature of interactions, and potential misinformation as a challenge for both ophthalmologists and their patients (35,83). Proactive engagement and vigilant oversight are essential to harness the full potential of SoMe in ophthalmology (84). Measuring ophthalmology trainees’ performance improvement and patients health literacy is vital (46,57,77,85-91).
Conclusions
The use of SoMe in HPE is supported by several learning theories; it encourages personal profiling, and learners’ knowledge co-creation, nurtures reflective, active, and social learning, and allows self-pace and choice over learning. SoMe widen outreach with mentors and diverse mentoring fields to embrace underrepresented and underserved learner communities. To maximize the beneficial effect and consolidate the role of SoMe in HPE, four critical aspects should be considered: the learning experience design, the role of educators, the selection of SoMe platforms, and the purpose of SoMe incorporation. SoMe can supplement and optimize learning experiences in HPE. Its integration in HPE should be used judiciously and adapted to the purpose intended, and should follow ethical principles. Its application needs to be continuously evaluated to establish its relevance and long-term impact on performance improvement.
In ophthalmology, SoMe has been shown to offer unprecedented opportunities for practice, research, advocacy, education, training, and patient engagement. While challenges such as ensuring reliable content quality and time management persist, proactive engagement, and quality policies with vigilant oversight are essential for maximizing the benefits of SoMe in HPE in general as well as in ophthalmology.
Acknowledgments
The authors acknowledge the Ophthalmology Foundation for offering the opportunity to explore the application of Social Media in Health Professions Education, which enabled the creation of one online module of the Teaching Skills Series (https://ophthalmologyfoundation.org/courses/teaching_skills/) and the present publication.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Eye Science for the series “Improving Teaching Skills in Ophthalmology”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://aes.amegroups.com/article/view/10.21037/aes-23-74/rc
Peer Review File: Available at https://aes.amegroups.com/article/view/10.21037/aes-23-74/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aes.amegroups.com/article/view/10.21037/aes-23-74/coif). The series “Improving Teaching Skills in Ophthalmology” was commissioned by the editorial office without any funding or sponsorship. K.G. served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Eye Science from November 2023 to October 2024. M.L. declares that a patent was submitted in an innovation project conducted at Tecnologico de Monterrey. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Greenhow C, Galvin SM, Staudt Willet KB. What Should Be the Role of Social Media in Education? Policy Insights from the Behavioral and Brain Sciences 2019;6:178-85. [Crossref]
- Greenhow C, Galvin S. Teaching with social media: evidence-based strategies for making remote higher education less remote. Information and Learning Sciences 2020;121:513-24. [Crossref]
- Cheston CC, Flickinger TE, Chisolm MS. Social media use in medical education: a systematic review. Acad Med 2013;88:893-901. [Crossref] [PubMed]
- Chan TM, Dzara K, Dimeo SP, et al. Social media in knowledge translation and education for physicians and trainees: a scoping review. Perspect Med Educ 2020;9:20-30. [Crossref] [PubMed]
- Chan TM, Gottlieb M, Sherbino J, et al. The ALiEM Faculty Incubator: A Novel Online Approach to Faculty Development in Education Scholarship. Acad Med 2018;93:1497-502. [Crossref] [PubMed]
- Sterling M, Leung P, Wright D, et al. The Use of Social Media in Graduate Medical Education: A Systematic Review. Acad Med 2017;92:1043-56. [Crossref] [PubMed]
- Guckian J, Utukuri M, Asif A, et al. Social media in undergraduate medical education: A systematic review. Med Educ 2021;55:1227-41. [Crossref] [PubMed]
- He B, Tanya SM, Costello F, et al. Navigating Personal and Professional Development Through Social Media in Ophthalmology. Clin Ophthalmol 2022;16:2263-74. [Crossref] [PubMed]
- Filipe HP, Tsui E, Marques JP, et al. “How to Teach Using Social Media” in the Teaching Skills Series of the Ophthalmology Foundation. Available online: https://ophthalmologyfoundation.org/courses/teaching_skills/
- Filipe HP, Tsui E, Marques JP, et al. “How to Teach Using Social Media” Available online: https://youtu.be/BsvWF1xmvXY?si=kyXQM8tKbbOtOaWz
- Bandura A. Self-Efficacy Mechanism in Human Agency. 1982. Available online: http://www.jennyarntzen.com/tsed321_951/current_files/pdf/Bandura1982.pdf
- Davitadze M, Ooi E, Ng CY, Zhou D, Thomas L, Hanania T, Blaggan P, Evans N, Chen W, Melson E, Arlt W, Kempegowda P. SIMBA: using Kolb's learning theory in simulation-based learning to improve participants' confidence. BMC Med Educ 2022;22:116. [Crossref] [PubMed]
- Boone T, Reilly AJ, Sashkin M. SOCIAL LEARNING THEORY Albert Bandura Englewood Cliffs, N.J.: Prentice-Hall, 1977. 247 pp., paperbound. Group & Organization Studies 1977;2:384-5. [Crossref]
- Boud D, Middleton H. Learning from others at work: communities of practice and informal learning. Journal of Workplace Learning 2003;15:194-202. [Crossref]
- Vygotsky LS. Mind in society: the development of higher psychological processes. Cambridge: Harvard University Press; 1978.
- Siemens G. Connectivism: A Learning Theory for the Digital Age. 2005. Available online: https://jotamac.typepad.com/jotamacs_weblog/files/Connectivism.pdf
- Halupa CM. Pedagogy, andragogy, and heutagogy. In: Transformative curriculum design in health sciences education. Hershey, PA: IGI Global, 2015:143-58.
- Blaschke LM. The pedagogy–andragogy–heutagogy continuum and technology-supported personal learning environments. In: Jung I. editor. Open and distance education theory revisited: Implications for the digital era. Singapore: Springer; 2019:75-84.
- Hase S, Kenyon C. From Andragogy to Heutagogy. ultiBASE; 2000. Available online: https://webarchive.nla.gov.au/awa/20010220130000/http://ultibase.rmit.edu.au/Articles/dec00/hase2.htm
- Nuttall J. Influences on the Co-construction of the Teacher Role in Early Childhood Curriculum: Some examples from a New Zealand childcare centre. International Journal of Early Years Education 2003;11:23-31. [Crossref]
- Wenger E. Communities of Practice: Learning, Meaning, and Identity. Higher Education from Cambridge University Press. 1998. Available online: https://www.cambridge.org/highereducation/books/communities-of-practice/724C22A03B12D11DFC345EEF0AD3F22A#overview
- Sargeant J, Curran V, Eva K, et al. CPD and the lifelong learning continuum for physicians. In: Future of Medical Education in Canada (FMEC). Theme 5, 2019.
- de Carvalho-Filho MA, Tio RA, Steinert Y. Twelve tips for implementing a community of practice for faculty development. Med Teach 2020;42:143-9. [Crossref] [PubMed]
- Koçak NG, Kaya S, Erol E. Social Media from the Perspective of Diffusion of Innovation Approach. The Macrotheme Review 2013;2:22-9.
- Gerstein J. Moving from Education 1.0 Through Education 2.0 Towards Education 3.0. In: Blaschke LM, Kenyon C, Hase S. editors. Experiences in Self-Determined Learning. South Carolina: CreateSpace Independent Publishing Platform; 2014:83-98.
- Toub D, Kostic M. Collaborative CME Using Web 2.0 Technologies. Alliance for CME Almanac. Vol 30, No 8, Aug 2008.
- Jessani NS, Hendricks L, Nicol L, et al. University Curricula in Evidence-Informed Decision Making and Knowledge Translation: Integrating Best Practice, Innovation, and Experience for Effective Teaching and Learning. Front Public Health 2019;7:313. [Crossref] [PubMed]
- Zafar Z, Umair M, Faheem F, et al. Medical Education 4.0: A Neurology Perspective. Cureus 2022;14:e31668. [Crossref] [PubMed]
- Filipe HP, Mack HG. Teaching through social media. Ann Eye Sci 2019;4:28. [Crossref]
- Lu D, Ruan B, Lee M, et al. Good practices in harnessing social media for scholarly discourse, knowledge translation, and education. Perspect Med Educ 2021;10:23-32. [Crossref] [PubMed]
- Kind T, Patel PD, Lie D, et al. Twelve tips for using social media as a medical educator. Med Teach 2014;36:284-90. [Crossref] [PubMed]
- Diug B, Kendal E, Ilic D. Evaluating the use of twitter as a tool to increase engagement in medical education. Educ Health (Abingdon) 2016;29:223-30. [PubMed]
- Boulos MN, Maramba I, Wheeler S. Wikis, blogs and podcasts: a new generation of Web-based tools for virtual collaborative clinical practice and education. BMC Med Educ 2006;6:41. [Crossref] [PubMed]
- Lahiri M, Moseley JL. Learning by Going Social: Do We Really Learn from Social Media? International Journal of Learning, Teaching and Educational Research. Vol. 11, No. 2:14–25.
- Joshi SM, Nagtode AH, Gosalia H, et al. Social media: A new-age educational platform for the millennial ophthalmologist! Indian J Ophthalmol 2023;71:2292-3. [Crossref] [PubMed]
- Eatz T, Al-Khersan H, Tanenbaum R, et al. Does social media have a place in ophthalmology practice? Expert Rev Ophthalmol 2021;16:329-31. [Crossref] [PubMed]
- Men M, Fung SSM, Tsui E. What's trending: a review of social media in ophthalmology. Curr Opin Ophthalmol 2021;32:324-30. [Crossref] [PubMed]
- Dave AD, Zhu D. Ophthalmology Inquiries on Reddit: What Should Physicians Know? Clin Ophthalmol 2022;16:2923-31. [Crossref] [PubMed]
- Sandalova E, Ledford JG, Baskaran M, et al. Translational Medicine in the Era of Social Media: A Survey of Scientific and Clinical Communities. Front Med (Lausanne) 2019;6:152. [Crossref] [PubMed]
- Latif MZ, Hussain I, Saeed R, et al. Use of Smart Phones and Social Media in Medical Education: Trends, Advantages, Challenges and Barriers. Acta Inform Med 2019;27:133-8. [Crossref] [PubMed]
- Nguyen AAK, Tsui E, Smith JR. Social media and ophthalmology: A review. Clin Exp Ophthalmol 2022;50:449-58. [Crossref] [PubMed]
- Tingley J, Allen RC, Barmettler A. #OculoplasticsandSocialMedia: a review of social media in oculoplastics and relevant subspecialties. Orbit 2022;41:141-9. [Crossref] [PubMed]
- Gheorghe CM, Purcărea VL, Gheorghe IR. Trick or treat: Social Media's dissemination power of ophthalmologic information in the pandemic context. Rom J Ophthalmol 2021;65:125-9. [Crossref] [PubMed]
- Alhalabi N, Salloum R, Aless A, et al. Messaging apps use in undergraduate medical education: The case of National Medical Unified Examination. Ann Med Surg (Lond) 2021;66:102465. [Crossref] [PubMed]
- Nathaniel GI, Adio O. How ophthalmologists and ophthalmologists-in-training in Nigeria use the social media. Niger J Med 2016;25:254-8. [Crossref] [PubMed]
- Greene II, Gold FE, Tan NE, et al. OphthoPods: An Analysis of the Educational Content and Changes of Ophthalmology Podcasts. J Acad Ophthalmol (2017) 2023;15:e248-57. [Crossref] [PubMed]
- Sugawara Y, Narimatsu H, Tsuya A, et al. Medical Institutions and Twitter: A Novel Tool for Public Communication in Japan. JMIR Public Health Surveill 2016;2:e19. [Crossref] [PubMed]
- Hussain I, Khan RA, Mahboob U, et al. Comparison of effectiveness of WhatsApp and Facebook as learning tool for the students of a medical college. J Pak Med Assoc 2020;70:1705-8. [Crossref] [PubMed]
- Qin VL, Chen AY, Bashir H, et al. Utilization of Instagram by Ophthalmology Residency Programs in the Era of COVID-19. Clin Ophthalmol 2023;17:1575-85. [Crossref] [PubMed]
- Tıskaoğlu NS, Seyyar SA. #Ophthalmology: Popular ophthalmology hashtags as an educational source for ophthalmologists, an Instagram study. Indian J Ophthalmol 2022;70:3247-52. [Crossref] [PubMed]
- Kaur K, Gurnani B. Commentary: Impact of social media applications like Instagram, Facebook, Twitter, and YouTube on ophthalmological education. Indian J Ophthalmol 2022;70:3253-4. [Crossref] [PubMed]
- Karataş ME, Karataş G. Evaluating the Reliability and Quality of the Upper Eyelid Blepharoplasty Videos on YouTube. Aesthetic Plast Surg 2022;46:754-9. [Crossref] [PubMed]
- Mangan MS, Cakir A, Yurttaser Ocak S, et al. Analysis of the quality, reliability, and popularity of information on strabismus on YouTube. Strabismus 2020;28:175-80. [Crossref] [PubMed]
- Yakobashvili D, Zhu A, Aftab OM, et al. Ophthalmology residency programs on social media. Int Ophthalmol 2023;43:4815-9. [Crossref] [PubMed]
- Park SSE, Akella SS, Moon JY, et al. Building Your Brand: Analysis of Successful Oculoplastic Surgeons on Social Media. Ophthalmic Plast Reconstr Surg 2020;36:582-9. [Crossref] [PubMed]
- Li J, Huang W, Gao J, et al. Impact of Mobile-Based Health Education on the Awareness and Knowledge of Glaucoma in Chinese Patients. Telemed J E Health 2019;25:455-61. [Crossref] [PubMed]
- Fouzdar Jain S, Eggleston C, Larson SA, et al. Is YouTube a Useful Tool for Trainees in Pediatric Cataract Surgery? J Pediatr Ophthalmol Strabismus 2022;59:200-3. [Crossref] [PubMed]
- Çetinkaya Yaprak A, Erkan Pota Ç. Assessment of the quality of information on treatment of keratoconus on YouTube. Int Ophthalmol 2022;42:1499-505. [Crossref] [PubMed]
- Balci AS, Cabuk KŞ, Topcu H, et al. Evaluation of the reliability, utility, and quality of the lid loading videos on YouTube. Int Ophthalmol 2023;43:2065-72. [Crossref] [PubMed]
- Kalayci M, Cetinkaya E, Suren E, et al. Are YouTube Videos Useful in Informing Patients about Keratoplasty? Semin Ophthalmol 2021;36:469-74. [Crossref] [PubMed]
- Sanguansak T, Morley KE, Morley MG, et al. Two-Way Social Media Messaging in Postoperative Cataract Surgical Patients: Prospective Interventional Study. J Med Internet Res 2017;19:e413. [Crossref] [PubMed]
- Kuçuk B, Sirakaya E. An Analysis of YouTube Videos as Educational Resources for Patients About Refractive Surgery. Cornea 2020;39:491-4. [Crossref] [PubMed]
- Garip R, Sakallioğlu AK. Evaluation of the educational quality and reliability of YouTube videos addressing eyelid ptosis surgery. Orbit 2022;41:598-604. [Crossref] [PubMed]
- Seyyar SA, Mete A, Tıskaoğlu NS. Evaluation of YouTube videos as a patient information source on intravitreal injection procedures. J Fr Ophtalmol 2022;45:748-55. [Crossref] [PubMed]
- Parmar UPS, Ichhpujani P, Chahal R, et al. Reliability of Ahmed glaucoma valve surgical videos for educational purposes. Int Ophthalmol 2023;43:3425-32. [Crossref] [PubMed]
- Chahal R, Jindal A, Parmar UPS, et al. Lifestyle Measures for Glaucoma Patients: An Objective Social Media Content Analysis. J Curr Glaucoma Pract 2023;17:141-8. [Crossref] [PubMed]
- Sakallıoğlu AK, Garip R. The reliability of trabeculectomy surgical videos on the internet for educational purposes in the changing world. Surgeon 2022;20:e371-7. [Crossref] [PubMed]
- Naseer S, Hasan S, Bhuiyan J, et al. Current Public Trends in the Discussion of Dry Eyes: A Cross-Sectional Analysis of Popular Content on TikTok. Cureus 2022;14:e22702. [Crossref] [PubMed]
- Schechet SA, Pandya HK, Mehta MC. Social media collaboration of retinal physicians: A 'Young Retina Forum' survey. Eur J Ophthalmol 2020;30:770-3. [Crossref] [PubMed]
- Lucatto LFA, Barbosa GCS, Prazeres JMB, et al. Use of surgical videos available on social media among retina surgeons: results of a vitreoretinal specialist survey. Arq Bras Oftalmol 2023; Epub ahead of print. [Crossref] [PubMed]
- Pakravan P, Gunawardene AN, Lai J, et al. What Are Patients Asking Online About Strabismus? An Analysis of the Strabismus Subreddit. J Binocul Vis Ocul Motil 2023;73:160-4. [Crossref] [PubMed]
- Tanyıldız B, Oklar M. Evaluating the quality, utility, and reliability of the information in uveitis videos shared on YouTube. Int Ophthalmol 2023;43:549-55. [Crossref] [PubMed]
- Altunel O, Sirakaya E. Evaluation of YouTube videos as sources of information about multifocal intraocular lens. Semin Ophthalmol 2021;36:423-8. [Crossref] [PubMed]
- Leitão Guerra RL. A perspective on retina education through social media. Int J Retina Vitreous 2020;6:44. [Crossref] [PubMed]
- Raffa L, Alattas K, Akeely O, et al. YouTube as a source of information for retinopathy of prematurity in the Arabic language. J Vis Commun Med 2023;46:30-6. [Crossref] [PubMed]
- Yildiz MB, Yildiz E, Balci S, et al. Evaluation of the Quality, Reliability, and Educational Content of YouTube Videos as an Information Source for Soft Contact Lenses. Eye Contact Lens 2021;47:617-21. [Crossref] [PubMed]
- Mahajan J, Zhu A, Aftab OM, et al. Educational quality and content of YouTube videos on diabetic macular edema. Int Ophthalmol 2023;43:1093-102. [Crossref] [PubMed]
- Bozali E, Yalinbas Yeter D. Assessment of YouTube videos as an information resource for keratoconus patients. J Fr Ophtalmol 2021;44:1545-52. [Crossref] [PubMed]
- Cheng T, Wang F, Barmettler A. #Oculoplastics: An Analysis of TikTok's Top Oculoplastics Content. Ophthalmic Plast Reconstr Surg 2022;38:452-7. [Crossref] [PubMed]
- Al Abbasi O, Al Taisan A, Alqahtani BS, et al. The Use of Social Media among Saudi Ophthalmologists: A Descriptive Cross-Sectional Study. Middle East Afr J Ophthalmol 2021;28:159-63. [Crossref] [PubMed]
- Sampige R, Rodgers EG, Huang A, et al. Education and Misinformation: Exploring Ophthalmology Content on TikTok. Ophthalmol Ther 2024;13:97-112. [Crossref] [PubMed]
- Mishra D, Nair AG, Verma L, et al. The perceived impact of webinars during the COVID.19 pandemic: A survey of ophthalmology trainees from India. Oman J Ophthalmol 2021;14:78-84. [Crossref] [PubMed]
- Mahjoub H, Prabhu AV, Sikder S. What are Ophthalmology Patients Asking Online? An Analysis of the Eye Triage Subreddit. Clin Ophthalmol 2020;14:3575-82. [Crossref] [PubMed]
- Seyyar SA, Tıskaoğlu NS. YouTube as a source of information on keratoconus: a social media analysis. Clin Exp Optom 2023;106:10-4. [Crossref] [PubMed]
- AlBloushi AF, Abouammoh MA. YouTube videos related to diabetic retinopathy: Are they good enough? J Fr Ophtalmol 2023;46:223-30. [Crossref] [PubMed]
- Al Hassan S, Bou Ghannam A. S Saade J. An Emerging Ophthalmology Challenge: A Narrative Review of TikTok Trends Impacting Eye Health Among Children and Adolescents. Ophthalmol Ther 2024;13:895-902. [Crossref] [PubMed]
- Gobeka HH, Gülyeşil FF, Yozgat Z, et al. Quality assessment and comparison of two- and three-dimensional YouTube videos as additional educational tools for cataract surgery: "METAVERSE". Ir J Med Sci 2023;192:2427-33. [Crossref] [PubMed]
- Altunel O, Sirakaya E. Evaluation of YouTube videos as sources of information about multifocal intraocular lens. Semin Ophthalmol 2021;36:423-8. [Crossref] [PubMed]
- Ozdemir Zeydanli E, Alkan AA. Era of "Dr. YouTube": Evaluation of YouTube Videos as a Valid Source for Patient Education on Keratoconus. Eye Contact Lens 2021;47:526-32. [Crossref] [PubMed]
- Vought R, Vought V, Herzog I, et al. EQIP Quality Assessment of Refractive Surgery Resources on YouTube. Semin Ophthalmol 2023;38:768-72. [Crossref] [PubMed]
- Watane A, Al-Khersan H, Kalavar M, et al. Self-Reported Social Media Use among Ophthalmology Residents. J Acad Ophthalmol (2017) 2021;13:e195-9. [Crossref] [PubMed]
Cite this article as: Filipe HP, Kostic M, Lopez M, Golnik K. Making the case for the evolving role of social media in health professions education and a literature review on the application of some in ophthalmology. Ann Eye Sci 2024;9:7.


