
More to it than meets the eye: a case report of incomitant esotropia in a child caused by a giant basilar aneurysm
Highlight box
Key findings
• This is the first pediatric case in Canada where a giant intracranial aneurysm (4.0 cm × 3.9 cm × 3.9 cm) was treated endovascularly.
What is known and what is new?
• While most pediatric esotropia stem from strabismus, it is crucial for physicians to differentiate atypical features that might indicate underlying organic causes.
• Surgical interventions for basilar aneurysms remain challenging and highly risky due to the anatomical complexity. Recent development of devices and techniques has led to reconstructive endovascular treatment with flow diverting stents.
What is the implication, and what should change now?
• Progressive incomitant esotropia and diplopia, the presence of myopia (rather than hyperopia), nystagmus and abnormal saccadic movements should be astutely recognized by clinicians as red flags when treating children with esotropia.
• Similar to adult cases, reconstructive endovascular treatment is a sensible approach for selected aneurysms in the pediatric population.
Introduction
Incomitant esotropia in children is frequently associated with an organic cause, including VI nerve palsy. Among children with VI nerve palsy, more than a third of the cases were due to intracranial space-occupying lesions (1). Though the incidence of cerebral aneurysm in children is low (2), this entity can cause devastating consequences.
Herein, we described a rare case of giant intracranial aneurysm in a child with a special focus on his ophthalmologic exams and radiologic findings. We further discussed salient red flag and atypical features of his esotropia that suggested an organic aetiology. The patient was treated promptly with the care of a multi-disciplinary team, and he made an excellent recovery in the long-term follow up. We present this article in accordance with the CARE reporting checklist (available at https://aes.amegroups.com/article/view/10.21037/aes-23-34/rc).
Case presentation
A previously healthy 8-year-old boy presented to ophthalmology emergency clinic with progressive esodeviation of the left eye and horizontal diplopia. His mother recalled a playground injury 4 months ago when the patient fell. He was initially seen by a physiotherapist and received cervical spine X-rays, which were deemed unremarkable. Approximately one month later, the child started to experience worsening esodeviation of the left eye with symptomatic horizontal diplopia. During this period, he denied headache, nausea or vomiting. He did not have any neurological or constitutional symptoms, and was able to carry out his daily routines.
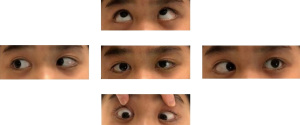
On exam, his visual acuity, pupillary reaction, intraocular pressure and colour vision were normal. His anterior and posterior segment exams were unremarkable as well. No swelling or pallor of the optic nerves were observed. His refractive errors were −3.00 diopters (D) in both eyes. His orthoptic exam demonstrated a left incomitant esotropia of 35 prism-diopter (PD) (Figure 1) with −3 abduction deficit, bilateral conjugated uniplanar horizontal nystagmus on left and right gazes, as well as a slow saccadic movement on left gaze.
Given these features in the context of a recent trauma, neuroimaging was performed with an initial hypothesis of a traumatic left VI nerve palsy, though the progressive nature was unusual. Magnetic resonance imaging (MRI) showed a giant basilar fusiform aneurysm (4.0 cm × 3.9 cm × 3.9 cm) extending from the vertebrobasilar junction to the level of the superior cerebellar artery origins (Figure 2A,2B). There was marked compression on the brainstem and the fourth ventricle, as well as crowding of the neural structures at the foramen magnum. The patient was admitted for urgent management. The multidiscipline team jointly discussed treatment options with the patient’s legal guardians who consented to the endovascular approach.

Catheter angiography was performed, which showed a fusiform aneurysm extending from immediately distal to the vertebrobasilar junction to the level of the superior cerebellar arteries where there was focal stenosis (Video 1). No intraluminal thrombus was noted and the circle of Willis was complete. Flow diversion was considered but not favoured given the age and anatomy. Balloon test occlusion (BTO) at the vertebrobasilar junction confirmed adequate flow reversal into the cerebellar arteries and distal basilar artery from the anterior circulation. Brainstem and sensorimotor evoked potentials were measured concomitantly and remained intact throughout. Following this, coil deconstruction of the aneurysmal segment was performed (Figure 3A,3B). Following the procedure, the patient was maintained on low dose anticoagulation with unfractionated heparin for 3 days to prevent accelerated intrasaccular thrombosis. One week after the procedure, he developed a new right VI cranial nerve palsy. MRI also showed focal diffusion restriction at the right facial colliculus and he was started on aspirin 81 mg daily.

Twelve months post-coiling, his bilateral VI cranial nerve palsies had resolved. He had excellent stereopsis with 20/20 best corrected visual acuity bilaterally. MRI at 1 year continued to demonstrate occlusion of the aneurysm with a reduction in size (3.4 cm × 3.1 cm × 3.1 cm) (Figure 3C).
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s parents for publication of this case report, any accompanying images, and the video. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Esotropia is a frequent reason of consult in pediatric ophthalmology, and is commonly seen in a general pediatric practice. Though the majority is strabismus in origin, physicians must distinguish atypical features that may suggest organic aetiologies. In this case, there were several red flags, including the progressive incomitant esotropia and diplopia, nystagmus and abnormal saccadic movements. These signs suggest an evolving VI nerve palsy from a pontine lesion.
One salient feature in this case lies in the size of the aneurysm: its maximal diameter (40 mm) is close to the 95th percentile of cerebral aneurysms (3). Of note, the pediatric population is more prone to giant cerebral aneurysms (defined as >25 mm in diameter), and often presents with neurologic deficits secondary to mass effects rather than intracranial hemorrhage (2). Untreated giant aneurysms are dangerous with mortality rates ranging from 65% to100% after 2 to 5 years of follow-up (4).
Surgical interventions for basilar aneurysms remain challenging and highly risky due to the anatomical complexity with the presence of cranial nerves, fine perforator vessels to the brainstem and a deep and narrow surgical field. Recent development of devices and techniques has led to reconstructive endovascular treatment with flow diverting stents (5). Compared to surgery, this endovascular approach has a significantly lower percentage of poor outcomes (11% vs. 30%) and fewer procedural complications in the adult literature (6). On the other hand, endovascular deconstructive techniques remain a viable option in the pediatric population, as demonstrated in this case, although care must be taken to select the appropriate candidate lesions to prevent catastrophic ischemic stroke.
To our knowledge, this is one of the largest pediatric intracranial aneurysms treated in Canada. Careful examination and thorough imaging study aided in its timely diagnosis and management. Given the rarity and complexity of this case, its long-term neurological and ophthalmologic outcomes remain unclear. We will continue to follow this patient with our multidisciplinary approach.
Conclusions
In summary, we present a rare case of unilateral VI nerve palsy due to giant basilar aneurysm in an 8-year-old child. When dealing with esotropia in children, one must recognize the red flags—the progressive incomitant esotropia and diplopia, the presence of myopia (rather than hyperopia), nystagmus and abnormal saccadic movements—which warrant timely neuroimaging to rule out dangerous aetiologies. Close ophthalmologic follow-ups are needed to optimize stereopsis and to prevent amblyopia.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://aes.amegroups.com/article/view/10.21037/aes-23-34/rc
Peer Review File: Available at https://aes.amegroups.com/article/view/10.21037/aes-23-34/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aes.amegroups.com/article/view/10.21037/aes-23-34/coif). T.E.Z. serves as an unpaid Editorial Board Member of Annals of Eye Science from April 2020 to March 2024. She is the editor for the Medical Education Column of AME Medical Journal. She also serves as a volunteer for Orbis Canada. And she received research grants from PSI foundation of Ontario and Fighting Blindness Canada. Both research grants were awarded for projects unrelated to the current manuscript. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s parents for publication of this case report, any accompanying images, and the video. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Harley RD. Paralytic strabismus in children. Etiologic incidence and management of the third, fourth, and sixth nerve palsies. Ophthalmology 1980;87:24-43. [Crossref] [PubMed]
- Sorteberg A, Dahlberg D. Intracranial Non-traumatic Aneurysms in Children and Adolescents. Curr Pediatr Rev 2013;9:343-52. [Crossref] [PubMed]
- Pico F, Labreuche J, Gourfinkel-An I, et al. Basilar artery diameter and 5-year mortality in patients with stroke. Stroke 2006;37:2342-7. [Crossref] [PubMed]
- Lawton MT, Abla AA, Rutledge WC, et al. Bypass Surgery for the Treatment of Dolichoectatic Basilar Trunk Aneurysms: A Work in Progress. Neurosurgery 2016;79:83-99. [Crossref] [PubMed]
- Kan P, Mokin M, Puri AS, et al. Successful treatment of a giant pediatric fusiform basilar trunk aneurysm with surpass flow diverter. J Neurointerv Surg 2016;8:e23. [Crossref] [PubMed]
- Sim SY, Chung J, Choi JH, et al. Basilar artery trunk aneurysm: clinical and angiographic outcomes of endovascular treatment. J Neurointerv Surg 2022;14:262-7. [Crossref] [PubMed]
Cite this article as: Zhou TE, Farinas CP, Kulkarni AV, Dirks P, Brandão LR, Muthusami P, Najm-Tehrani N. More to it than meets the eye: a case report of incomitant esotropia in a child caused by a giant basilar aneurysm. Ann Eye Sci 2023;8:20.


