
Subjective refractions determined by Dyop® and LogMAR chart as fixation targets
Introduction
Visual impairment is an important condition affecting approximately 285 million people of all ages worldwide (1). In China, over 50 million people suffer from various levels of visual impairment (2). The World Health Organization (WHO) estimated uncorrected refractive error and cataract are associated with 42% and 33% of visual impairment respectively globally (1). About 153 million people are visually impaired from uncorrected refractive errors (3) although prevalence of refractive errors varies across age groups, genders, ethnicities, and regions (4-6). Spectacle correction significantly improves the vision for those with uncorrected refractive error (7). In Hong Kong, the vision of about 70% of elderly people could be corrected by distance spectacles (8,9).
Visual acuity charts with optotypes, including letters, numbers, Tumbling E, and Landolt C, are used to measure visual acuity and refractive error. The logarithm of the minimum angle of resolution (LogMAR) acuity chart has the advantage of standardizing the letter size in each line and is generally considered as accurate and repeatable, but may take more time for the measurement. Several studies have compared various visual acuity charts with the LogMAR chart (10-12). In addition, people who are illiterate may have difficulties with the conventional visual acuity measurement.
Dyop®, a new dynamic optotype designed by Hytowitz (13), is a rotating and segmented visual stimulus method for visual acuity and refractive error measurement. The image diameter is adjusted by angular arc width and calibrated with the viewing distance to measure the acuity threshold (Figure 1) (13). The acuity measurement starts by presenting the subject with large spinning Dyop® targets. The diameter of targets continues to reduce until the subject can no longer perceive any motion of the targets. The acuity endpoint is determined by the minimum stimulus area of perception of the Dyop® segment motion. Thus, Dyop® offers an alternative for measurement of visual acuity and refractive error which is independent of culture, literacy, and language. A pilot study, conducted by Harris et al to validate visual acuity measurements with the Dyop® system, reported that measurement result was comparable to Sloan letters, although the comparison was between dynamic and static acuity (14,15). The purpose of the current study is to compare refractive error measurement using the LogMAR E and Dyop® acuity charts. We present the following article in accordance with the STROBE reporting checklist (available at https://aes.amegroups.com/article/view/10.21037/aes-22-17/rc).

Methods
Subject recruitment
Fifty subjects aged 18 or above with habitual aided visual acuity better than 6/12 in both eyes and without any history of ocular disease were recruited in the Optometry Clinic of the School of Optometry, The Hong Kong Polytechnic University. Subjects with Parkinson’s disease and/or Alzheimer’s disease were excluded, as these respondents may have difficulties in motion perception (16,17).
All the subjects received an information sheet about the research study and written consents were obtained. The study was approved by the Human Subjects Ethics Committee of The Hong Kong Polytechnic University (No. HSEARS20170215006) and the study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Subjective refraction
Objective refraction of all subjects was measured using an autorefractor (NIDEK ARK 510A, Japan) under closed-view conditions. The result was used as the starting point of the refraction procedures. The starting optotype size was 0.3 LogMAR in each chart. The subjective refraction in both eyes was measured with the same phoropter and two different visual acuity charts.
3-meter LogMAR E chart
The LogMAR E chart (Figure 2), produced by The Hong Kong Polytechnic University, was placed 3 m away from the subject. A conventional subjective refraction protocol was used, which included best sphere measurement, use of duochrome, astigmatism measurement by Jackson Cross Cylinder method, and binocular balancing by fogging and alternate occlusion. The refraction protocol was performed according to Clinical Procedures in Primary Eye Care (18). The best corrected visual acuity in LogMAR was recorded for both eyes.
Dyop® acuity chart (Figure 3)
The chart, provided by Allan Hytowitz (13), was displayed on a monitor placed 6 m away from the subject. The high contrast black and white Dyop® acuity test target was used with the rotating figure appearing on a 50 per cent grey background. Two Dyop® targets were presented: one rotating and one static. The Dyop® target equivalent to 0 logMAR rotated at 40 revolutions per minute. Dyop® acuity was collected in arc minutes, representing the visual angle of the outer diameter of the circular optotype. The smallest diameter for rotation detection was determined by reducing the size of the Dyop® moving target until the subject could not perceive any motion of the target. The refractive power was deemed to reach the smallest Dyop® diameter. The refraction protocol was as follows:
- With the objective refraction in place, the sphere power was adjusted until the Dyop® acuity was reduced to the smallest diameter for rotation detection;
- The axis of astigmatism was rotated until the Dyop® acuity was reduced to the smallest diameter for rotation detection;
- The power of astigmatism was adjusted until the Dyop® acuity was reduced to the smallest diameter for rotation detection;
- Binocular balancing by fogging and alternate occlusion;
- The best corrected Dyop® in arc minutes was recorded for both eyes.
To convert Dyop® in arc minutes to LogMAR units, a graph was plotted using the data provided by the Dyop® acuity test with an equation [LogMAR acuity = 0.7674 × In (Dyop® arc minute) − 1.5602].
The order of the two measurements was determined randomly and the measurements taken 5 min apart. The best corrected visual acuity and time spent on each subjective refraction measurement was recorded. The time spent on subjective refraction was measured from best sphere determination to binocular balancing with best corrected visual acuity. All measurements were collected by the principal investigator (RS) in the same room with the same illumination. RS has been a practicing optometrist for over 10 years.
Thibo’s notation
Thibo’s notation was used to represent the refractive error obtained from the subjective refraction (19). The sphero-cylindrical combinations were divided into spherical equivalent (M) (sphere + cylinder/2) and two Jackson crossed cylinders at 180° [J0 = (cylinder/2) cos2β] and 45° [J45= (cylinder/2) sin2β)]. β was the axis of the cylinder power obtained from the subjective refraction. These three components are independent and could be used to compare the results from the two acuity charts.
Statistical analysis
The visual acuity data were presented in LogMAR units with E chart and arc minutes with Dyop®. Thibo’s Notation was used to represent the refractive error. Mann-Whitney U test was used to compare the differences of measurements between the two acuity charts. Bland-Altman plots were used to determine the limits of agreement between the two charts. A P value <0.05 was considered statistically significant. Data were analyzed using IBM SPSS Statistics version 23 software (IBM Corp., Armonk, NY, USA).
Results
This study recruited fifty subjects, aged 44.94±12.07 years, of whom 62% (31/50) were female. The mean differences of M, J0, and J45 measured by the two visual acuity charts were compared between the two eyes. As non-significant difference was found between eyes (P>0.05) for all of components, only the data from one eye (right eye, after binocular balance) was used in the analysis.
Spherical equivalent (M)
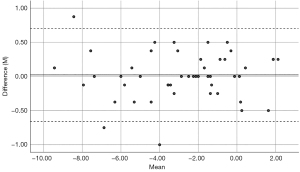
There was no significant difference between the two charts (z=−0.05, P=0.96) with means of −2.88±2.85 D (range −9.37 to +2.25 D) with the LogMAR E chart and −2.90±2.85 (range −9.50 to +2.00 D) with Dyop®. The mean difference of M between the LogMAR E chart and Dyop® acuity test was 0.02±0.35 D, with upper and lower limits of agreement at 0.70 and −0.66 D, respectively. Bland-Altman plots showed the difference in M was within 95 per cent of agreement across the refractive errors measured (Figure 4).
Component J0 and J45
The mean value of J0 was 0.05±0.40 D (range −0.88 to 0.96 D) using LogMAR E chart and 0.03±0.41 D (range −0.86 to 0.86 D) with Dyop®, whilst that of J45 was 0.01±0.33 D (range −0.80 to 1.29 D) with LogMAR E chart and 0.01±0.31 D (range −0.72 to 1.41 D). As for spherical equivalent, there was no significant difference in J0 (z=−0.28, P=0.78) and J45 (z=−0.66, P=0.51) between the two charts. The mean difference of J0 and J45 between the LogMAR E chart and Dyop® acuity test was 0.03±0.12 and 0±0.11 D, with the upper and lower limits of agreement at 0.26, −0.21 and 0.22, −0.21 D, respectively. Bland-Altman plots showed the difference in J0 and J45 were within 95 per cent of agreement for the refractive errors measured (Figures 5,6).


Subjective refraction duration
The duration of completing the subjective refraction of both eyes was recorded. The measurement was faster (t=4.46, P<0.05) with Dyop® (mean =419.90±91.17 seconds, range 209 to 586 seconds) than LogMAR E chart (mean =452.04±74.71 seconds, range 313 to 600 seconds). The higher standard deviation could be due to motion perception difference.
Discussion
Before using the dynamic optotype for subjective refractive error measurement, it is important to determine if visual acuity measurement by Dyop® is comparable with that of the LogMAR E chart. A previous study revealed that the mean difference of visual acuity measured by Dyop® and LogMAR E chart was 0.05±0.07 LogMAR unit, which did not reach statistical significance (20). With comparable visual acuity measurement, this study aimed to investigate the refractive error measurement with a dynamic acuity chart by comparing the results measured with a conventional LogMAR E chart. Thibo’s notation (M, J0, and J45) was used to represent the refractive error measurement. There was only 0.02±0.35 D mean difference in the spherical equivalence (M), 0.03±0.12 and 0±0.11 D in the cross cylinder (J0 and J45). In optometry practice, prescriptions for spectacles or contact lenses are usually graduated in steps of 0.25D. Therefore, the mean differences of refractive error measured by the two charts were both statistically and clinically insignificant. These results were similar to another study comparing subjective refractive error measurement with Dyop® and the Snellen letter chart (21), in which the refractive error measured with the two methods were comparable. However, the refractive errors of the subjects were not evenly distributed in this study (spherical equivalent findings ranged from −9.37 to +2.25). Further investigation was needed to study the subjects with higher hyperopia.
The current study also recorded the time of refractive error measurement with the two acuity charts, with Dyop® measurement taking 32 seconds less time than using the LogMAR E chart. Although there are only four choices of answer indicating the direction of letter E in the LogMAR chart, subjects may still need some time to perceive the clarity of the target during refractive error measurement. In contrast, there were only two possible answers when using Dyop®, i.e., the target was rotating or not rotating, which may explain the faster measurement with Dyop® acuity chart. The difference was even more pronounced for comparison of Dyop® with the Snellen letter chart, with Dyop® measurement time only half of that using the Snellen chart (21). During refractive error measurement with either LogMAR E chart or Snellen letter chart, the practitioner assesses if the subject has responded to the target correctly and needs time to obtain the best acuity by adjusting the lens power. In contrast, the practitioner only needs to adjust the lens power to reach the point that the subject can perceive a non-moving target with Dyop®, allowing the end point of refractive error measurement to be reached faster.
The study does have the limitation the observer was not blinded to the first refraction results before comparison. This can be improved by having more than one investigator with insignificant inter-investigator variation. In addition, all the subjects in the current study had habitual aided visual acuity better than 6/12. Thus, the agreement of refractive error measurement between the two acuity charts among those with more impaired vision remains uncertain. Further research is needed to investigate the agreement of refractive error measurement of Dyop® for subjects with more severely reduced visual function, e.g., those with amblyopia, glaucoma, and macular degeneration.
Conclusions
Subjective refractive error measured by the Dyop® acuity chart was comparable to the traditional LogMAR E chart, but use of the Dyop® acuity chart is slightly faster. It can be considered as an alternative method in subjective refraction measurement.
Acknowledgments
We thank Mr. Allan Hytowitz for providing the Dyop® acuity programme and Dr. Maureen Boost for the technical editing.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://aes.amegroups.com/article/view/10.21037/aes-22-17/rc
Data Sharing Statement: Available at https://aes.amegroups.com/article/view/10.21037/aes-22-17/dss
Peer Review File: Available at https://aes.amegroups.com/article/view/10.21037/aes-22-17/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://aes.amegroups.com/article/view/10.21037/aes-22-17/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All the subjects received an information sheet about the research study and written consents were obtained. The study was approved by the Human Subjects Ethics Committee of The Hong Kong Polytechnic University (No. HSEARS20170215006) and the study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol 2012;96:614-8. [Crossref] [PubMed]
- Xu T, Wang B, Liu H, et al. Prevalence and causes of vision loss in China from 1990 to 2019: findings from the Global Burden of Disease Study 2019. Lancet Public Health 2020;5:e682-91. [Crossref] [PubMed]
- Resnikoff S, Pascolini D, Mariotti SP, et al. Global magnitude of visual impairment caused by uncorrected refractive errors in 2004. Bull World Health Organ 2008;86:63-70. [Crossref] [PubMed]
- Vitale S, Sperduto RD, Ferris FL 3rd. Increased prevalence of myopia in the United States between 1971-1972 and 1999-2004. Arch Ophthalmol 2009;127:1632-9. [Crossref] [PubMed]
- Vitale S, Ellwein L, Cotch MF, et al. Prevalence of refractive error in the United States, 1999-2004. Arch Ophthalmol 2008;126:1111-9. [Crossref] [PubMed]
- Sawada A, Tomidokoro A, Araie M, et al. Refractive errors in an elderly Japanese population: the Tajimi study. Ophthalmology 2008;115:363-370.e3. [Crossref] [PubMed]
- Ferraz FH, Corrente JE, Opromolla P, et al. Influence of uncorrected refractive error and unmet refractive error on visual impairment in a Brazilian population. BMC Ophthalmol 2014;14:84. [Crossref] [PubMed]
- Michon JJ, Lau J, Chan WS, et al. Prevalence of visual impairment, blindness, and cataract surgery in the Hong Kong elderly. Br J Ophthalmol 2002;86:133-9. [Crossref] [PubMed]
- Fung MM, Yap MKh, Cheng KK. Correctable visual impairment among people with diabetes in Hong Kong. Clin Exp Optom 2010;93:453-7. [Crossref] [PubMed]
- Tong L, Saw SM, Chan ES, et al. Screening for myopia and refractive errors using LogMAR visual acuity by optometrists and a simplified visual acuity chart by nurses. Optom Vis Sci 2004;81:684-91. [Crossref] [PubMed]
- Chaikitmongkol V, Nanegrungsunk O, Patikulsila D, et al. Repeatability and Agreement of Visual Acuity Using the ETDRS Number Chart, Landolt C Chart, or ETDRS Alphabet Chart in Eyes With or Without Sight-Threatening Diseases. JAMA Ophthalmol 2018;136:286-90. [Crossref] [PubMed]
- Lim LA, Frost NA, Powell RJ, et al. Comparison of the ETDRS logMAR, 'compact reduced logMar' and Snellen charts in routine clinical practice. Eye (Lond) 2010;24:673-7. [Crossref] [PubMed]
- Hytowitz A. Dyop®. Available online: https://chart2020.com/dyop (Retrieved 6 September 2021).
- Harris P, Gryczynski J. Validation of the Dyop Acuity Test. Proceedings of the Annual meeting of The Association for Research in Vision and Ophthalmology, Seattle WA., 2015. Available online: https://iovs.arvojournals.org/article.aspx?articleid=2333791 (Retrieved 13 July 2022).
- Harris P. Validation of the Dyop Visual Acuity Measure (A Pilot Study). Proceedings of the Annual meeting of American Academy of Optometry, Seattle WA., 2013. Available online: https://chart2020.com/wp-content/uploads/2017/10/2015_ARVO_Harris-2.pdf (Retrieve 13 July 2022).
- Armstrong RA. Oculo-visual dysfunction in Parkinson’s disease. J Parkinsons Dis 2015;5:715-26. [Crossref] [PubMed]
- Fernandez R, Monacelli A, Duffy CJ. Visual motion event related potentials distinguish aging and Alzheimer's disease. J Alzheimers Dis 2013;36:177-83. [Crossref] [PubMed]
- Elliott D. Clinical Procedures in Primary Eye Care. Philadelphia: Elsevier Saunders, 2021.
- Thibos LN, Wheeler W, Horner D. Power vectors: an application of Fourier analysis to the description and statistical analysis of refractive error. Optom Vis Sci 1997;74:367-75. [Crossref] [PubMed]
- Sum WMR, Woo GC. Comparison of distance visual acuity measurement between dynamic optotype and LogMAR E charts. Chin J Exp Ophthalmol 2021;39:534-37.
- Sanni IO. Subjective comparison between Dyop® and Snellen refractions. Optom Vis Perf 2020;8:202-13.
Cite this article as: Sum RW, Woo GC. Subjective refractions determined by Dyop® and LogMAR chart as fixation targets. Ann Eye Sci 2022;7:34.




