
Folded technique of self-adherent wrap improves clinical outcomes for wounds after orbital tumour extirpation: a single-center, prospective randomized controlled trial
Introduction
Eye bandaging is a common treatment for wounds following complex eye surgery that is used to arrest haemorrhage and reduce swelling (1). If eye haemorrhage or oedema is not successfully managed, it can lead to the development of a variety of complications and ultimately the loss of visual function. Self-adherent wrap is widely used to create consistent appropriate pressure to control oedema (2,3). In addition to decreasing oedema, self-adherent wrap is also advantageous in that it is self-adherent, secure, protective, and adaptable to any size but does not adhere to underlying tissues (4).
The classic compression technique (1) with self-adherent wrap is a standard procedure for wounds after orbital tumour extirpation. It effectively arrests haemorrhaging and reduces swelling by maintaining pressure over the eye pad (1). However, using the classic compression technique (1) also results in pressure outside of the affected eye (e.g., on the forehead and below the ear) that can cause discomfort because of the repeated circuits of the bandage. In addition, repeated circuits on the forehead and below the ear are not useful for controlling haemorrhaging or oedema in the affected eye. Moreover, neck flexion should be repeated multiple times (7 times) when using the classic technique in patients receiving general anaesthesia, which may increase the severity of postoperative upper airway obstruction (5). Recently, several publications have described the usage of self-adherent wraps on the hands and legs (2,3), but still less attention has been focused on its evidence-based application on eyes.
The folded compression technique of self-adherent wrap has been applied to the wounds of patients who underwent orbital tumour extirpation while under general anaesthesia. The bandage is repeated on the cheek and up over the affected eye to the forehead instead of circuiting around the head and below the ear. The application of this technique provides the same number of overlaps in the interface pressure on the affected eye and less overlaps outside of the affected eye. It may reduce pressure on the forehead and below the ear without influencing pressure on the eye, reduce the frequency at which neck flexion must be performed, and increase patient acceptance and compliance with therapy. To further explore the effects of these two methods of applying self-adherent wraps on the eye, we prospectively evaluated interface pressure measurements on the affected eye and outside of the affected eye and discomfort scores in 128 consecutive patients who underwent orbital tumour extirpation with general anaesthesia. We present the following article in accordance with the CONSORT reporting checklist (available at http://dx.doi.org/10.21037/aes-20-123).
Methods
Design
This was a single-centre, prospective, randomized, controlled, noninferiority study (ClinicalTrials.gov identifier: NCT03415490). The flow of clusters and participants through the trial is shown in Figure 1. The trial included 128 consecutive patients who underwent anterior approach for orbital tumour surgery between January and April 2018 in Zhongshan Ophthalmic Center. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Zhongshan Ophthalmic Center, Sun Yat-sen University (2016MEKY006) and informed consent was taken from all individual participants.
A sample size of 64 patients per treatment group (128 total) was planned to provide 80% power to determine noninferiority based on the mean interface pressure on the affected eye of the folded technique of 1.40 mmHg and 1.43 in the classic technique by our preliminary experiments, using a two-sample noninferiority test with an equivalence margin of 0.1, an alpha of 0.025 and an estimated common standard deviation (SD) of 0.14 by using SAS software (SAS Institute, Cary, NC, USA).
Study visits were scheduled on day 1 (visit 1/baseline), day 2 (visit 2, operation day), and day 3 (visit 3, 24 hours after the operation).
Participants
Participants were screened before the trial by an experienced doctor. The following inclusion criteria were applied: (I) monocular anterior approach for orbital tumour surgery and the requirement an eye bandage after surgery; (II) age ≥16 years; and (III) general anaesthesia administration during ophthalmic surgery.
The exclusion criteria were as follows: previous trauma or surgery of the eyes, previous experience with or a history of an allergic reaction to using self-adherent wraps, and an inability to communicate (including impaired sensorium).
Data collection
Random assignment was done by a research assistant via a central computer system at Orbital Diseases Clinical Centre of Zhongshan Ophthalmic Center by a computer-generated random number code. Patients were randomly assigned in a 1:1 ratio with a block size of four (known only to the statistician). At the baseline visit (day 1), patients were randomly divided into the Group A (classic technique) or Group B (folded technique) of applying self-adherent wraps after surgery. Participants and the surgeon were blinded to treatment assignment until the point of implementation. On day 2 (operation day), interventions were applied by the same experienced bandager for awake patients 10 minutes after surgery was completed. For each of the two methods of self-adherent wraps, measurements of interface pressure were obtained at four points near the eye 10 minutes after bandage application. After 1 minute of recording, the patients were asked to fill out a numerical analogue scale of discomfort with scores ranging from 0 to 10, in which 0 indicated no discomfort and 10 indicated the worst imaginable discomfort. This test has been confirmed to be sensitive and reliable (6). Postoperative events, such as upper airway obstruction, increasing fever, nausea, vomiting, bleeding, swelling or decreased visual acuity, were reported for 24 hours (day 3).
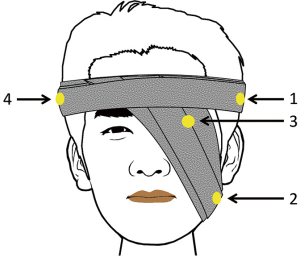
Measurements of interface pressure were obtained using a small portable sub-bandage pressure-monitoring device (Sensor ZNHBM, Zhongnuo, China) for each of the two tested methods of self-adherent wraps application. The sensitivity and the error of the pressure-monitoring device are 2.0±0.1 mV/V and ±0.05%F·S separately. Measurements were obtained at four points on or near the eye (Figure 2). The pressure probe was placed above the ear of the affected side (“point 1”), below the ear of the affected side (“point 2”), on the affected eye (“point 3”), and above the ear of the non-affected side (“point 4”). Pressure was sequentially recorded starting after the self-adherent wrap bandage was applied while the patient was lying down. Three successive measurements were acquired at each point, and the mean value of the three measurements was considered as the pressure value.
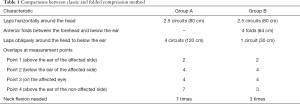
As shown in Figure 3, the classic compression technique (1) consisted of wrapping a piece of self-adherent wrap around the patient’s head starting with the opened end on the forehead above the affected eye. The bandage was then firmly but not tightly wrapped around the head twice. After the second circuit, the bandage was brought below the ear, up over the affected eye and around the head of the non-affected side and then wrapped around the head in the same manner four times. The bandage was then brought around the head once.

When using the folded technique to apply a piece of self-adherent wrap, the procedure began in a manner similar to the classic compression technique described above. After the second circuit, the bandage was brought on the cheek and up over the affected eye to the forehead, where it was passed between the eyebrows but not wrapped around the head. Instead, the bandage was folded and then first passed back on the cheek of the affected side then back to the forehead for a total of four times. Finally, the bandage was wrapped completely around the head once. Table 1 displays the comparison between folded and classic compression technique.
Full table
Analysis
The primary outcome was the interface pressure on the affected eye (“point 3”). Secondary outcomes were the interface pressure at three other points outside of the affected eye, including above (“point 1”) and below (“point 2”) the ear of the affected side, above the ear of the non-affected side (“point 4”), and discomfort scores.
Interface pressure and numerical analogue scale scores were compared between groups using independent sample t-test in patients to identify discomfort points and differences in interface pressure at each pressure point. The level of significance was set at P<0.05. SPSS 19.0 (IBM Corp., Armonk, NY, USA) was used for all statistical analyses.
Results
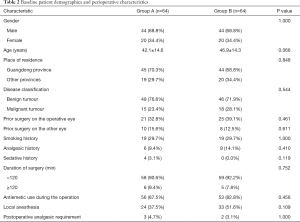
Figure 1 depicts the CONSORT flow of participants through the trial. A total of 130 individuals were assessed for the eligibility of the study, of these 2 disqualified for meeting exclusion criteria. A total of 128 consecutive patients who agreed to participate in the study were enrolled. There were no losses or exclusions following randomisation. The overall median age was 47.0 (range, 16.0–80.0) years. There were 88 male and 40 female patients. The two groups were well balanced in terms of baseline demographics and perioperative characteristics (Table 2).
Full table
Interface pressure
Table 3 displays the interface pressure for each measurement point and the numerical analogue scale of discomfort scores for the classic and folded techniques of applying self-adherent wraps. The overall mean pressure was 0.91 mmHg and ranged from a mean pressure of 1.37 mmHg on the affected eye (“point 3”) to 0.54 mmHg below the ear on the affected side (“point 2”). The pressure was always higher surrounding the affected eye than that at the other three measurement points outside of the affected eye (all P≤0.001).

Full table
The pressure placed on the affected eye (“point 3”) was similar between the classic and folded techniques (P=0.480). The pressures at the other three points outside of the affected eye (“points 1, 2, and 4”) were significantly (P=0.041, 0.019, and 0.047, respectively) higher when the classic technique was used than when the folded technique was used.
Discomfort scores and complications
All patients showed slight swelling, regardless of which technique was used. There were no episodes of fever, nausea, vomiting, or retrobulbar haemorrhage in any patient, and no permanent loss of vision or afferent pupillary defects were observed. Discomfort scores were higher in the classic technique group than in the folded technique group (2.93±0.30 vs.1.52±0.19, P≤0.001). No upper airway obstruction was observed all both groups.
Discussion
The objective of this study was to perform a unified investigation of the classic and folded techniques of applying self-adherent wrap bandages on the wounds of patients who underwent anterior approach for orbital tumour surgery. Self-adherent wrap is used to create consistent, appropriate pressure to control oedema (2,3). However, while several previous publications have described the use of self-adherent wraps on the hands and legs (2-4,7,8), few evidence-based studies have explored its use on the eye. In this paper, we present the results of our study of self-adherent wrap application on the eye.
Eye bandages are commonly used to treat patients who have undergone oculoplastic surgery. The bandages are used to arrest haemorrhage and reduce swelling (1). However, when using the classic compression technique (1), the pressure outside of the affected eye (on the forehead and below the ear) can cause discomfort because the bandage is repeatedly wrapped around the head and ears. Additionally, repeated circuits on the forehead and below the ear do not control eye haemorrhage or oedema of the affected eye. Moreover, repeated neck flexion during the classic compression technique may increase the severity of upper airway obstruction in patients treated with general anaesthesia (9). Our aim was to prospectively gather valid data to compare the folded and classic compression techniques of applying self-adherent wrap on the eye in patients who underwent orbital tumour extirpation.
It is difficult to draw conclusions from different application techniques on initial pressures delivered by bandages (10). In order to minimise the variables that could influence the findings, bandages were applied by the same experienced bandager to the same operative procedure (orbital tumour extirpation), and each bandaging technique was carried out in a separate experiment. Participants and the surgeon were blinded to treatment assignment until the point of implementation. All of the above make precautions meaningful analysis possible.
Our results show that noninferiority was demonstrated for the primary endpoint, the interface pressure on the affected eye was similar between the classic and folded techniques (P=0.480). However, superiorities were achieved for the secondary efficacy endpoints. Pressure on the other three points outside of the affected eye (i.e., above the ear of the affected side, below the ear of the affected side and above the ear of the non-affected side) was significantly (P=0.041, 0.019, and 0.047, respectively) higher when the bandages were applied using the classic technique than when the folded technique was used. Although the data showed that the pressure placed on the four points was slightly lower when using the folded technique than when using the classic technique, no episodes of complications, such as fever, nausea, vomiting or retrobulbar haemorrhage, were observed in any patient. These results indicate that it may be preferable to use the folded technique to apply self-adherent wraps because it exerts less pressure on the forehead and below the ear and did not influence pressure on the affected eye.
On the other hand, patients who were treated using the classic technique reported significantly higher discomfort scores than those who were treated using the folded technique (P≤0.001). This increase was very likely because the amount of pressure outside of the affected eye (the forehead and below the ear) was higher. The pressure would cause discomfort, which was defined as “sensation other than pain” and included nausea, vomiting, headache, and dizziness that were reported by the patients who underwent complex surgery (11).
The main technical difference between the two techniques is the number of overlaps on the forehead and below the ear of the affected side. The number of overlaps is correlated with the amount of applied pressure (12,13), with a higher number of overlaps being associated with higher interface pressure. In our study, the classic and folded techniques exerted an identical amount of pressure on the affected eye, and both overlapped this pressure point 4 times. When the bandage was applied using the classic technique, in which more overlaps are applied to the points outside of the affected eye, the pressure values were significantly higher than those obtained using the folded technique (P=0.041, 0.019, and 0.047, respectively). Similarly, it was previously reported that 50% overlap corresponds to two layers of bandage, while 66% overlap corresponds to three layers of bandage (12).
Moreover, because of its high postoperative incidence of adverse respiratory rate (9), repeated neck flexion (7 times) which was applied while using the classic compression technique, may increase the severity of upper airway obstruction in patients treated with general anaesthesia (5). It is known that with neck flexion, anaesthesia state can cause posterior displacement of the epiglottis, narrowing of the oropharynx, and widening of the laryngeal vestibule comparing with the conscious (14). Moreover, adverse respiratory events are a leading cause of postoperative morbidity and mortality, especially in patients undergoing major surgery and those treated with general anaesthesia (9) or paediatric anaesthesia (15). Hence, if the folded technique were applied instead of the classic technique, the required frequency and duration of postoperative neck flexion would be markedly reduced to 3 times while the patient is recovering from general anaesthesia, and the probability of adverse respiratory events would therefore be lower.
Our study had some limitations. First, the bandager was not blinded as each technique had a distinct appearance and method of application. The observation period was short, as the interface pressure of the bandage and discomfort scores were recorded only soon after the bandage application, and postoperative events were reported only for 24 hours after surgery. Moreover, all bandages were applied only by the same experienced bandager to the same operative procedure to prevent large variations in the bandage application. As a result, the learning curve for operators was not studied in this study. However, it would be interesting to evaluate the variation of the two different techniques between different bandagers.
Conclusions
In conclusion, our findings showed that the folded technique to apply self-adherent wrap is superior to the classic technique in the wounds of orbital tumour extirpation patients in lowering the interface pressure outside of the affected eye and patient discomfort, without influencing the interface pressure on the affected eye. Furthermore, no operative complications were reported with this technique and the probability of adverse respiratory events may be lower.
Acknowledgments
Funding: This work was supported by the National Natural Science Foundation of China (81700875, 81870689, 81670887) and the Sun Yat-sen University Clinical Research 5010 Program, China (2014014).
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at http://dx.doi.org/10.21037/aes-20-123
Data Sharing Statement: Available at http://dx.doi.org/10.21037/aes-20-123
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes-20-123). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Zhongshan Ophthalmic Center, Sun Yat-sen University (2016MEKY006) and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Stevens S. How to apply an eye pad, shield, and bandage. Community Eye Health 2010;23:56. [PubMed]
- Glassey N, Phillips M. Comparison of the effect of two application methods of self-adherent wrap (CobanTM) on range of motion in the hands of healthy subjects. Hand Therapy 2011;6:42-4. [Crossref]
- Schuren J, Bernatchez SF, Tucker J, et al. 3M Coban 2 Layer Compression Therapy: Intelligent Compression Dynamics to Suit Different Patient Needs. Adv Wound Care (New Rochelle) 2012;1:255-8. [Crossref] [PubMed]
- Ward RS, Reddy R, Brockway C, et al. Uses of Coban self-adherent wrap in management of postburn hand grafts: case reports. J Burn Care Rehabil 1994;15:364-9. [Crossref] [PubMed]
- Regli A, von Ungern-Sternberg BS. Diagnosis and Management of Respiratory Adverse Events in the Operating Room. Curr Anesthesiol Rep 2015;5:156-67. [Crossref]
- Price DD, Bush FM, Long S, et al. A comparison of pain measurement characteristics of mechanical visual analogue and simple numerical rating scales. Pain 1994;56:217-26. [Crossref] [PubMed]
- Smith TO, Hazelden S, Parker L, et al. The use of CobanTM compression bandage following below-knee free-flap surgery. Int J Nurs Pract 2012;18:604-9. [Crossref] [PubMed]
- Enos L, Lane R, MacDougal BA. Brief or new: the use of self-adherent wrap in hand rehabilitation. Am J Occup Ther 1984;38:265-6. [Crossref] [PubMed]
- Xará D, Santos A, Abelha F. Adverse respiratory events in a post-anesthesia care unit. Arch Bronconeumol 2015;51:69-75. [Crossref] [PubMed]
- Lee AJ, Dale JJ, Ruckley CV, et al. Compression therapy: effects of posture and application techniques on initial pressures delivered by bandages of different physical properties. Eur J Vasc Endovasc Surg 2006;31:542-52. [Crossref] [PubMed]
- Korn BS, Kikkawa DO, Vasani SN, et al. Evaluation of patient comfort with outpatient orbital surgery. Orbit 2007;26:19-22. [Crossref] [PubMed]
- Thomas S. Measuring sub-bandage pressure. J Wound Care 2000;9:491-2. [PubMed]
- Moffatt C. Variability of pressure provided by sustained compression. Int Wound J 2008;5:259-65. [Crossref] [PubMed]
- Kobayashi M, Ayuse T, Hoshino Y, et al. Effect of head elevation on passive upper airway collapsibility in normal subjects during propofol anesthesia. Anesthesiology 2011;115:273-81. [Crossref] [PubMed]
- von Ungern-Sternberg BS, Boda K, Chambers NA, et al. Risk assessment for respiratory complications in paediatric anaesthesia: a prospective cohort study. Lancet 2010;376:773-83. [Crossref] [PubMed]
Cite this article as: Ye H, Lian X, Chen R, Zhu Y, Huang J, Chen H, Xie L, Guo W, Yang H. Folded technique of self-adherent wrap improves clinical outcomes for wounds after orbital tumour extirpation: a single-center, prospective randomized controlled trial. Ann Eye Sci 2021;6:13.



