
Ophthalmology residency training program at the University of Montreal
Historical overview
In 1975, Michel Mathieu became the head of the newly autonomous Department of Ophthalmology at the University of Montreal. Mathieu’s growing reputation as a skilled clinician and researcher attracted excellent candidates to the department (1). Under his direction, Suzanne Véronneau-Troutman became the first resident and, subsequently, the first female ophthalmic surgeon at University of Montreal. Her immense contribution to the field of strabismus later gained worldwide appreciation, as recognized by the annual American Academy of Ophthalmology award named after her (2). Mathieu’s work, and that of his recruits, led to major advances in the fields of corneal transplantation, retinal degenerations, electroretinography, and ophthalmic surgical instrumentation (3). This rich history of clinical excellence and innovation still inspires the department’s academic mission today, which is to provide high quality ophthalmology training to medical students, residents, and subspecialty fellows, as well as to foster a platform for innovative fundamental and clinical vision science research. The department now includes more than 90 clinicians and researchers spanning across all ophthalmologic sub-specialties. Its Ophthalmology Residency Training Program is one of the four accredited in the Province of Quebec, and has grown over the years to become the largest in Canada, training five residents per year.
Admission criteria
In Canada, medical students apply to residency in the last of their four- or five-year undergraduate medical training through the Canadian Resident Matching Service (CaRMS)—a national, independent organization. It ensures a standardized and transparent application process, and uses an algorithm to match applicants’ and programs’ ranking lists. Candidates to our program are short-listed after review of their clinical evaluation forms, curricula vitae, and letters of intent, and are then invited to an interview. The interview model is validated and includes four 15-minute stations with two interviewers per station, including six faculty members and two co-chief residents (4). Each station is designed to assess one to two of the CanMED roles defined by the Royal College of Physicians and Surgeons of Canada (RCPSC), namely communication, collaboration, erudition, management, health advocacy, professionalism, and medical expertise. These reflect the applicant’s potential as future residents and, later, ophthalmologists (5). Although an applicant’s past experiences and training plays an important role, great weight is attributed to their motivation and eagerness to learn. Medicals schools from the Province of Quebec represent the main source of candidates to the program, although the number of applicants from other Canadian provinces has been growing over the last years.
High volume training centers
Admitted residents rotate through four sites: University of Montreal Hospital Center (CHUM), Maisonneuve-Rosemont Hospital (HMR), Sainte-Justine Hospital (HSJ), and Sacré-Coeur Hospital of Montreal (HSCM). The University of Montreal Hospital Center (CHUM) is a recently inaugurated mega-hospital complex with state-of-the-art installations housing a large Ophthalmology Department. The department includes 35 ophthalmologists and 75 other ocular health care professionals who see more 78,000 patients and perform over 10,000 surgeries per year (6). The residents are exposed to all sub-specialties at this center, including the largest vitreoretinal surgery and neuro-ophthalmology services in the province, the only ocular oncology service in Montreal, and super-specialized expertise in the field of the Boston type I keratoprosthesis implantation, among others (7). Maisonneuve-Rosemont Hospital (HMR) fosters the University of Montréal Ophthalmology University Center (CUO), a designation underlying its national leading position in vision health care and research. Over 500 patients are seen at Maisonneuve-Rosemont Hospital (HMR) daily across all ophthalmology subspecialties. The center was the first to offer Descemet membrane endothelial keratoplasty, the latest and most selective corneal transplantation technique, in Quebec, and is one of the two centers in Canada to implant the Argus retinal prosthesis (8,9). Pediatric ophthalmology exposure is obtained at Sainte-Justine Hospital (HSJ), one of the largest pediatric centers in Canada and North-America. Residents rotate through general pediatric ophthalmology, as well as through specialized clinics in pediatric cornea, glaucoma, retina, uveitis, oculoplastics and neuro-ophthalmology (10). Exposure to trauma and globe rupture cases occurs mainly in the fifth year of training when residents rotate through the Sacré-Coeur Hospital of Montreal (HSCM), a Level-One trauma center.
Residency curriculum
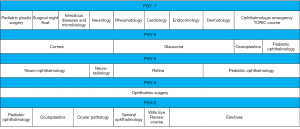
The ophthalmology curriculum is dictated by the Royal College of Physicians and Surgeons of Canada (RCPSC) standards and is submitted to regular accreditation reviews (11). The first year of residency consists of foundational clinical training with rotations in internal medicine and specialties such as infectious diseases, neurology and plastic surgery (Figure 1). Exposure to ophthalmology begins at the end of this first year with the six-week Toronto Ophthalmology Resident Introductory Course (TORIC), which includes didactic teaching, wet labs and dissection sessions. During junior years (2 and 3), residents rotate through the different sites to acquire a solid learning foundation in all subspecialty disciplines. Surgical training is gradually introduced in these years with oculoplastics and strabismus surgeries. Fourth year is entirely dedicated to surgical ophthalmology. Residents focus on cataract surgery training, achieving between 300 and 400 cases per resident, but also have the option to learn basic glaucoma and corneal surgeries, on an interest-driven basis. Surgical training is supported by two wet lab installations equipped with modern operative microscopes and phacoemulsification machines at the University of Montreal Hospital Center (CHUM) and Maisonneuve-Rosemont Hospital (HMR). The use of the Eyesi®, a high-end virtual reality simulator for intraocular surgery, allows residents to refine their dexterity prior to real-life surgeries. In operating rooms, cutting-edge installations like the intraoperative anterior-segment optical coherence tomography and the NGENUITY® 3D Visualization System complement residents’ training. The fifth and final year completes the clinical training with oculoplastic, pediatric and ocular pathology rotations, and provides time for electives, allowing residents to pursue their interests and prepare for potential fellowship opportunities.
Research during training is strongly encouraged, and supported with protected time (one day per month throughout residency) and dedicated funds. Residents are required to complete at least one project. Those interested can enroll in the University’s Clinician-Investigator Program and complete a combined master’s or doctorate degree. Trainees can choose among the numerous fundamental and clinical research mentors of the department and a wide range of research areas, including ocular neuro-vascular disorders, corneal transplantation and regeneration, retinal regeneration, telemedicine and ophthalmic public health care (12).
One dedicated academic half-day and one rounds meeting are committed weekly. Monthly conferences given by invited clinicians and researchers are held within the department and attract worldwide visiting professors. Local written and oral examinations are held once a year in addition to the Ophthalmic Knowledge Assessment Program (OKAP) examinations. The final licensing exam is provided by the Royal College of Physicians and Surgeons of Canada (RCPSC), and includes a written and an oral portion. In the last seventeen years, the success rate on this licensing exam was 100%.
After residency
Following post-graduate education, residents have the option of practicing general ophthalmology or extending their training by pursuing fellowships. In the last five years, 15/25 (60%) graduating residents pursued subspecialty training and the remaining 10/25 (40%) started comprehensive ophthalmology practices.
Conclusions
The Ophthalmology residency training program at the University of Montreal is an excellent post-graduate medical program that has distinguished itself, over the years, as a platform for renewal and innovation in ophthalmology, through research, academia and community service. It graduates highly-trained ophthalmologists for Quebec and Canada and strong academicians who will ensure sustainability of the program, and conduct ground-breaking research to consolidate the department’s leading position on a national and international scale.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Tianwei Ellen Zhou) for the series “Medical Education Column” published in Annals of Eye Science. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2020.02.02). The series “Medical Education Column” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- d’Ophtalmologie FdM-D. Études médicales postdoctorales - résidence. Available online: https://ophtalmologie.umontreal.ca/etudes/etudes-medicales-postdoctorales-residence/. Published 2019. Accessed September 22, 2019.
- Ophthalmology Wi. Suzanne Véronneau-Troutman Award. 2019.
- Goulet D. L'Hôpital Maisonneuve-Rosemont: une histoire médicale, 1954-2004. Septentrion, 2004.
- Hamel P, Boisjoly H, Corriveau C, et al. Using the CanMEDS roles when interviewing for an ophthalmology residency program. Can J Ophthalmol 2007;42:299-304. [Crossref] [PubMed]
- Canada RCoPaSo. CanMEDS: Better standards, better physicians, better care. Available online: http://www.royalcollege.ca/rcsite/canmeds/canmeds-framework-e. Published 2019. Accessed.
- CHUM. L’ophtalmologie: un département de pointe au service des patients. Chumagazine Montreal 2018;9:9-13.
- CHUM. Le CHUM innove: voir l'œil en 3d pour mieux l'opérer. Available online: https://www.chumontreal.qc.ca/nouvelles/Voir-l-oeil-en-3d. Published 2018. Accessed.
- l’Est-de-l’Île-de-Montréal Ciudsedssd. Axes d’excellence. Available online: https://ciusss-estmtl.gouv.qc.ca/propos/axes-dexcellence/sante-de-la-vision. Published 2019. Accessed.
- Ruel-Manseau A. Révolution de la greffe de cornée au Québec. La Presse +. Available online: http://plus.lapresse.ca/screens/c4d12d58-d93c-4ae7-bd73-4cc44ed511f5%7C_0.html. Published 2015. Accessed.
- SAINTE-JUSTINE C. Département d'ophtalmologie. Available online: https://www.chusj.org/fr/a-propos/Directions-Departements/Departements/Ophtalmologie. Published 2014. Accessed.
- (RCPSC) RCoPaSoC. Specialty Training Requirements in Ophthalmology. Available online: http://www.royalcollege.ca/rcsite/documents/ibd/ophthalmology-str-e.pdf. Published 2019. Accessed.
- d’Ophtalmologie FdM-D. Activités de recherche. Available online: https://ophtalmologie.umontreal.ca/recherche/activites-de-recherche/. Published 2019. AccessedNovember 17, 2019.
Cite this article as: Antaki F, Bostan C, Goodyear E. Ophthalmology residency training program at the University of Montreal. Ann Eye Sci 2020;5:10.


