Regaining birth weight and predicting ROP—a prospective, pilot study
Introduction
Retinopathy of prematurity (ROP) is the leading cause of preventable blindness in infants world-wide. Countries like India and other middle-income countries are believed to be suffering from the third epidemic (1,2). ROP screening is performed by using screening criteria of birth weight (BW) and or gestational age (GA) although there are several other systemic risk factors that may contribute in different measures to the outcome of ROP in an infant (3-5).
In India, infants born < or equal to 2,000 grams and/or < or equal to 34 weeks of GA are screened before they turn 30 days old (6). However, GA assessment in a vast majority of rural mothers is inaccurate leading to discrepancies in enrolment into the screening program. BW assessment is a more robust and accurate measurement, and is reliably available in most babies, even in non-institutional and rural deliveries (7). This has led to BW becoming the single most important criteria for enrollment into the ROP screening program.
With the national emphasis on BW, the quest to develop simple tools that may be able to predict “at-risk” babies has been a constant endeavor. One innovative, low-cost method of risk stratification is by capturing serial postnatal weight gain, which is a surrogate for insulin-like growth factor 1 (IGF-1) (8-11). Predictive models have demonstrated accurate ROP risk assessment and a reduction in the proposed number of ROP examinations. These include, WINROP, a computer-based algorithm that identifies cumulative deviations from the expected weight gain, ROPScore—a spreadsheet-based equation, and CHOP ROP, a normogram based model that uses a single equation with BW and GA and weight gain (12,13). Limitations of these models include a precise estimate of sensitivity and poor generalizability of these models to countries with higher BW and GA infants that require treatment, like in India (14). Most of these models require serial, daily weight measurements up to 6 weeks or more after birth. In the Indian scenario, where infants are discharged from the neonatal intensive care unit (NICU) early, this is not always feasible, since there is poor compliance for follow-up after discharge of the baby.
In this pilot study we attempt to correlate the day of life when the baby regains its initial loss of body weight after birth with the final outcome of ROP. We noted that mothers remembered this day with accuracy, because of a cultural belief that a child who has regained its BW has a better chance of survival. The primary outcome of the study was to evaluate the correlation between the duration (in days) required to regain BW with the development of ROP. As a secondary outcome, we used this duration to stratify risk, which has the potential to influence the follow-up schedule.
Methods
Preterm, Asian Indian infants who were enrolled for ROP screening in the Karnataka Internet Assisted Diagnosis of Retinopathy of Prematurity (KIDROP) tele-ROP program, were enrolled into the study. All babies fulfilled the national screening guidelines of ≤2,000 grams and/or ≤34 weeks of gestation. Those infants who lacked complete hospital records, or were unsure of the weight change measures or who were lost to follow-up before the final ROP status could be documented, were excluded from the study.
Sixty-eight consecutively enrolled infants who fulfilled the study criteria were included for the analysis. Chart records of weight (grams) measured daily using a digital weighing scale, were accessed while the baby was admitted in the respective NICU. In discharged cases (6/68 babies), the mother was contacted telephonically and asked to get the infant weighed at a local center and the value was noted. These weight measures were noted until the baby “regained their respective BWs” rounded off to the closest whole integer. This “age of regaining BW” value was correlated with the eventual retinal status of all enrolled babies. While we prospectively and independently collected the daily BWs of these infants from the nursing charts, the mothers were also separately asked to recall the date of regaining lost weight at the end of the study period.
The outcome was divided into no ROP, ROP which regressed spontaneously (type 2 ROP), and ROP which required treatment (type 1) as per the ICROP classification (15). Computing these values, a risk score was estimated to predict which babies would develop the disease. IBM SPSS ver23 and MedCalc were used for statistical analysis and plots. One-way ANOVA with Bonferroni correction was applied to test the mean difference between the groups (no ROP, type 2 and type 1).
The study fulfilled the requirement of the Institute Research Board (IRB) and was approved by the Institute Ethics Committee (IEC). Written, informed consent was obtained from the parents or legal guardians of all the study recruits.
Results
Of the 68 patients enrolled in the study, 33 infants (48.5%) did not have any ROP, 20 infants (29.4%) had type 2 ROP and 15 infants (22.1%) had type 1 ROP.
The mean BW of the study cohort was 1,270±340 grams and the mean GA was 31±2 weeks. The mean difference in BW, GA and number of days to regain BW was found to be significantly different between the three groups (P<0.001). On applying Bonferroni correction, the mean BW was comparable between no ROP and type 2 (P=0.08) and between type 1 and type 2 (P=1.00) and was significantly different between no ROP and type 1 (P=0.013). The mean GA was significantly different between no ROP vs. type 2 and no ROP vs. type 1 (P<0.001) comparable between type 2 and type 1 (P=1.00).
Days required to regain BW
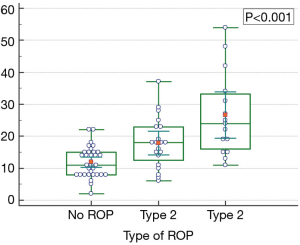
All 68 mothers (100%) were able to accurately recall the date on which their infant had regained the lost weight. The mean number of days for the No ROP group to regain BW was 11.9±4.6 days, for the type 2 ROP group was 17.9±7.9 days and for the type 1 ROP group was 26.6±12.9 days respectively. To reduce the influence of outliers on the mean values, we performed a robust fit analysis and found they were comparable (no ROP 11.9 days, type 2 ROP 17.6 days and type 1 ROP 24.8 days respectively). The number of days to regain BW was significantly different between no ROP vs. type 1 and no ROP vs. type 2 and type 1 vs. type 2 (P<0.001).
Risk stratification
The mean and distribution of the age at regaining BW is depicted in Figure 1. In this study cohort, no baby developed any stage ROP if it regained its BW in 6 or less days and all babies who took 37 or more days to regain their weight developed type 1 ROP. We used the 95% confidence intervals of the groups to develop a generalizable risk stratification. Those babies who regained their BW within 10 days were at the least risk of developing any stage ROP. Those who took 11–20 days were at moderate risk and those who took more than 21 days were at the highest risk of developing type 2 or type 1 ROP.
Discussion
ROP has become an important public health concern in middle-income countries. India and China lead the world in the number of preterm infants with the former accounting for over 3.5 million annually (16). With an overall increase in survival, improved neonatal care delivery especially in the rural hospitals, improved awareness about ROP, and more recently a spurt in medical negligence cases against institutes not providing timely and appropriate ROP screening or referral, the quest for an ideal screening program has become a policy concern for the federal and state governments in India (17).
As with any public health initiative, a program’s success is measured by the enrolment of those who are “at risk”. ROP screening is based on an “opportunistic screening” model with the NICU being the focus. Measures to detect “risk factors” that can “predict” which babies eventually progress to developing ROP are constantly being researched. This leads to modifications in the screening protocol to address regional concerns. For example, despite the clinical unlikelihood of ROP being present or detected within 1 week of life, a recent study from India showed that by screening babies before discharge from the NICU (even if a few days old), the yield of enrolment, detection and follow-up were better than if the conventional “30-day-rule” was followed (18).
Cultural beliefs and social norms in neonatal care may influence ROP screening. In this study, we evaluated a culturally prevalent parameter with its outcome on ROP, i.e., the timing of regaining BW after a baby had lost its initial weight after birth. Culturally, a baby who has regained his or her weight is considered to be more likely to survive than a baby who did not. The recall value of this date was exploited in this study, especially amongst mothers. We found that all mothers accurately recalled the date on which their infants had regained this weight in our study.
Predictive models including WINROP, ROPScore and CHOP ROP are limited by their sensitivity, lack of generalizability especially in non-Caucasian populations and often require accurate daily weight recordings for over 6 weeks or more before the alarms for ROP risk can get flagged (12-14). The advantages of these tools however remain in their long track record, validated computer based algorithms and high sensitivity in the population it was originally tested in (13). Whereas it may be argued that in our study we too relied on daily weight recordings, there are two fundamental differences. Firstly, our recording stopped when the baby regained its BW which was considerably shorter than what is required in the other tools. Secondly, since we saw that the recall of the mothers was very accurate, eliciting the daily weight record may not be necessary. However, it needs to be evaluated in a larger community setting before this conclusion is made.
The limitations of the study include its relatively small sample size of 68 infants. Besides, the number of babies developing any stage and treatment requiring ROP were higher in proportion than that is prevalent in the community. This bias is likely because we only enrolled infants who had daily weight records accurately measured which was possible mostly in those admitted for longer periods in the NICU. These were most often the sickest infants who were most likely to develop ROP. However, the babies were enrolled from over 35 NICU’s across our screening network, and are less likely to have center specific admission bias. Secondly, we did not assess other co-morbidities in the perinatal period. Though they have the potential to impact ROP outcome, these were deliberately left out of the study to allow assessment of regaining BW as an independent and simple tool to determine ROP risk. Finally, our cohort comprised of a homogenous Asian Indian ethnicity and needs to be validated in other ethnic groups.
The national ROP screening guidelines in India recommends that all babies ≤2,000 grams, be “first” screened before “30 days of life”. The recommended first screening date is between 3–4 weeks for babies born >1,200 grams and between 2–3 weeks for those born below 1,200 grams (6). Our results may help in stratifying risk before they are initiated into the screening program. If a baby regains its weight within 10 days of life, the risk of developing ROP appears to be the least. If the baby takes more than 21 days, the risk is the highest. Hence the ROP specialist and the neonatologist could use the weight regaining date as an additional risk factor while enrolling a baby into the program. Those infants at higher risk could also be advised closer follow-up. This will also act as a good tool to counsel parents especially if they are discharged within 1 month of birth.
This pilot study demonstrates a simple tool that is culturally acceptable, easily accessible and can be recorded without any additional cost to the parents or the treating hospital.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aes.2017.03.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study fulfilled the requirement of the Institute Research Board (IRB) and was approved by the Institute Ethics Committee (No. ECR/187/Inst/Kar/2013:C/2015/05/09) and written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gilbert C, Rahi J, Eckstein M, et al. Retinopathy of prematurity in middle-income countries. Lancet 1997;350:12-4. [Crossref] [PubMed]
- Gilbert C, Fielder A, Gordillo L, et al. Characteristics of infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development: implications for screening programs. Pediatrics 2005;115:e518-25. [Crossref] [PubMed]
- Knezević S, Stojanović N, Oros A, et al. Analysis of risk factors in the development of retinopathy of prematurity. Srp Arh Celok Lek 2011;139:433-8. [Crossref] [PubMed]
- Fierson WMAmerican Academy of Pediatrics Section on Ophthalmology. American Academy of Ophthalmology; et al. Screening examination of premature infants for retinopathy of prematurity. Pediatrics 2013;131:189-95. [Crossref] [PubMed]
- . Retinopathy of prematurity: guidelines for screening and treatment. The report of a Joint Working Party of The Royal College of Ophthalmologists and the British Association of Perinatal Medicine. Early Hum Dev 1996;46:239-58. [PubMed]
- Pejaver RK, Bilagi AP, Vinekar A. National Neonatology Foundation’s Evidence Based Clinical Practice Guidelines 2010. Retinopathy of Prematurity (NNF India, Guidelines) 2010:253-62.
- Vinekar A, Avadhani K, Dogra M, et al. A novel, low-cost method of enrolling infants at risk for Retinopathy of Prematurity in centers with no screening program: the REDROP study. Ophthalmic Epidemiol 2012;19:317-21. [Crossref] [PubMed]
- Löfqvist C, Andersson E, Sigurdsson J, et al. Longitudinal postnatal weight and insulin-like growth factor I measurements in the prediction of retinopathy of prematurity. Arch Ophthalmol 2006;124:1711-8. [Crossref] [PubMed]
- Smith LE. IGF-1 and retinopathy of prematurity in the preterm infant. Biol Neonate 2005;88:237-44. [Crossref] [PubMed]
- Raghuveer TS, Bloom BT. A paradigm shift in the prevention of retinopathy of prematurity. Neonatology 2011;100:116-29. [Crossref] [PubMed]
- Löfqvist C, Hansen-Pupp I, Andersson E, et al. Validation of a new retinopathy of prematurity screening method monitoring longitudinal postnatal weight and insulinlike growth factor I. Arch Ophthalmol 2009;127:622-7. [Crossref] [PubMed]
- Piermarocchi S, Bini S, Martini F, et al. Predictive algorithms for early detection of retinopathy of prematurity. Acta Ophthalmol 2017;95:158-64. [Crossref] [PubMed]
- Hutchinson AK, Melia M, Yang MB, et al. Clinical Models and Algorithms for the Prediction of Retinopathy of Prematurity: A Report by the American Academy of Ophthalmology. Ophthalmology 2016;123:804-16. [Crossref] [PubMed]
- Binenbaum G. Algorithms for the prediction of retinopathy of prematurity based on postnatal weight gain. Clin Perinatol 2013;40:261-70. [Crossref] [PubMed]
- International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol 2005;123:991-9. [Crossref] [PubMed]
- United Nations. Born Too Soon. The Global Action Report on Preterm Birth. 2012. Accessed August 15, 2016. Available online: http://www.who.int/pmnch/media/news/2012/201204_borntoosoon-report.pdf
- Civil Appeal No. 8065 OF 2009. Accessed August 15, 2016. Available online: http://supremecourtofindia.nic.in/FileServer/2015-07-02_1435823185.pdf
- Vinekar A, Jayadev C, Mangalesh S, et al. Initiating Retinopathy of Prematurity Screening before Discharge from the Neonatal Care Unit: Effect on Enrolment in Rural India. Indian Pediatr 2016;53:S107-S111. [PubMed]
Cite this article as: Vinekar A, Mangalesh S, Mallavarapu M, Jayadev C, Sharma P, Shetty B. Regaining birth weight and predicting ROP—a prospective, pilot study. Ann Eye Sci 2017;2:50.